By Peter Loftus and Jonathan D. Rockoff
Combining new immune-boosting cancer drugs with each other or
with older drugs improved survival in patients with lung cancer,
compared with traditional chemotherapy, new studies found.
The benefits of the new cocktails, which include immunotherapies
from Merck & Co. and Bristol-Myers Squibb Co., come with high
price tags because they combine already expensive drugs, a trend
that worries doctors even as they welcome advances in treating lung
cancer, the deadliest type of tumor.
"We're talking about people living significantly longer than
they would otherwise live," said Dr. Nasser Altorki, cardiothoracic
surgeon at Weill Cornell Medicine and NewYork-Presbyterian, who
wasn't involved in the studies. "It's not going to be cheap, and I
really don't know how we as a society deal with that."
Companies in recent years have introduced new drugs that harness
patients' immune systems to fight tumors, such as Merck's Keytruda
and Bristol's Opdivo. When used alone, the drugs have been shown to
improve patient survival in cancers including melanoma and certain
types of lung cancer. Keytruda and Opdivo each cost about $13,500
monthly per patient.
They don't work for every patient, however, so companies have
been racing to test whether combining immunotherapies with each
other or with older drugs could further improve patient
survival.
Lung cancer is the leading cancer killer, causing about 1.69
million deaths globally in 2015, according to the World Health
Organization. The American Cancer Society estimates about 234,030
new cases of lung cancer will be diagnosed in the U.S. this year,
and about 154,050 Americans will die from the disease this
year.
The New England Journal of Medicine published online the results
of two new studies of lung-cancer combination therapies Monday, and
researchers are presenting them at the annual meeting of the
American Association for Cancer Research in Chicago.
In one of the studies, researchers said adding Keytruda to two
chemotherapy drugs prolonged overall survival in patients with the
most common type of lung cancer. The study of more than 600
patients started in 2015, and the Keytruda-containing combination
reduced the risk of death by 51% compared with the chemotherapies
alone.
An estimated 69% of patients getting the combination were alive
12 months after the start of treatment, versus 49% for those on
chemotherapy.
The combination came with side effects, including an increased
risk of kidney injury. About 13.8% of patients taking the
combination discontinued therapy because of adverse events,
compared with 7.9% in the control arm.
Analysts were watching the trial as a test of Merck's strategy
of focusing much of its development budget on Keytruda.
The Keytruda combination provides "meaningful survival
differences and something better than chemotherapy," said Dr. Leena
Gandhi, director of thoracic medical oncology at NYU Langone
Health's Perlmutter Cancer Center and lead author of the study.
Dr. Altorki of Weill Cornell said he thinks the study results
will prompt doctors to prescribe the combination more widely as a
first-line treatment for patients newly diagnosed with advanced
lung cancer.
Based on the results, Merck plans to seek European regulatory
approval to market the combination there, said Roger Perlmutter,
Merck's head of research and development. The U.S. Food and Drug
Administration approved the combination last year, based on an
earlier, smaller study.
The second study looked at a combination of two Bristol-Myers
immunotherapies, Opdivo and Yervoy, compared with chemotherapy in
untreated non-small cell lung-cancer patients.
The study focused on 299 subjects whose tumors were biopsied,
sequenced and found to have a high number of genetic mutations,
known as tumor mutational burden.
Subjects who received Bristol's two immunotherapies were 42%
less likely to have their cancer progress after a year of treatment
than subjects getting chemotherapy, a measure known as
progression-free survival. Tumors hadn't progressed in 43% of the
immunotherapy subjects, compared with 13% of those who received
chemotherapy, one year after treatment started.
The researchers are still awaiting results on whether the
combination improved overall survival compared with chemotherapy in
the study.
Fouad Namouni, who heads cancer-drug development at Bristol,
said the results suggest the immunotherapy combination would
benefit certain lung-cancer patients more than chemotherapy.
"We are redefining the utility of chemotherapy in the standard
of care" of lung-cancer patients, he said. "Chemotherapy has
toxicity and is active in the very short term, when immunotherapy
can have a long-term efficacy."
About 31.3% of patients taking the Bristol immunotherapies
experienced high-severity side effects, compared with 36.1% of
those getting chemotherapy.
Write to Peter Loftus at peter.loftus@wsj.com and Jonathan D.
Rockoff at Jonathan.Rockoff@wsj.com
(END) Dow Jones Newswires
April 16, 2018 09:44 ET (13:44 GMT)
Copyright (c) 2018 Dow Jones & Company, Inc.
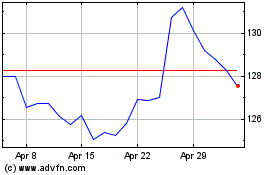
Merck (NYSE:MRK)
Historical Stock Chart
From Mar 2024 to Apr 2024
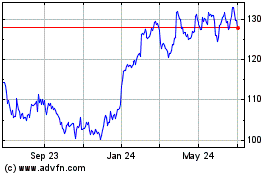
Merck (NYSE:MRK)
Historical Stock Chart
From Apr 2023 to Apr 2024