By Rolfe Winkler
Susan Baker volunteered for Johnson & Johnson's vaccine
trial to seek protection from Covid-19. For the same reason, she
may drop out of the study.
The nurse practitioner at a North Carolina hospital has treated
Covid-19 patients. She takes care of people at high risk, including
dialysis patients and her husband and father, both of whom have
medical conditions. If she catches the virus and spreads it to
anyone vulnerable, "I don't know if I could forgive myself," she
said.
That is why Ms. Baker may drop out of J&J's vaccine trial.
She took an antibody test indicating she received a placebo instead
of the actual vaccine in the study. With positive early results for
vaccines from Pfizer Inc. and Moderna Inc. pointing toward use in
the U.S. possibly within weeks, she wants to be first in line to
get one, though she previously agreed to stick with the study so it
could fully vet J&J's injection.
"Anything that could potentially protect you, you want so
desperately right now," the 42-year-old said.
Authorization of the most advanced vaccine candidates would mark
a turning point in the fight against Covid-19. Yet it might also
set back the effort, compromising ongoing vaccine trials, including
Pfizer's and Moderna's, by prompting volunteers to quit.
Researchers scheduled two-year trials for the leading vaccines.
They didn't plan to tell the volunteers whether they got a shot or
placebo until a study ends. Subjects agreed to the terms upon
signing up.
Yet Ms. Baker and others say it is unfair to deny them vaccines
once they become available.
She and more than 100 other vaccine-study subjects recently
wrote the U.S. Food and Drug Administration asking it to encourage
companies to tell them if they got a placebo and are eligible for
an authorized vaccine.
The subjects are free to leave their trials at any time,
drug-research experts say. Yet early departures could undermine the
studies by hindering the collection of data needed to fully assess
how safe the inoculations are and how long they protect against the
virus.
"Frankly, people should not have gone into this study who didn't
feel they could wait," said Arnold Monto, a University of Michigan
health researcher who heads the panel of experts that will advise
the FDA about authorizing Covid-19 vaccines.
Dr. Monto expressed hope the issue would be rendered moot
because many volunteers who received a placebo aren't likely to be
eligible for scarce vaccine supplies for some time.
The dilemma strikes at a larger, more enduring problem with
medical testing: Many trial participants volunteer for a chance at
early access to a Covid-19 vaccine, not to further science. Yet
researchers conduct the studies to determine whether they can
recommend an experimental treatment to the broader community.
"The small group on the placebo wants access [to a vaccine] at
the time of authorization; the whole world wants more rigorous
safety and efficacy data, which means keeping people on a placebo,"
said Jennifer Miller, a Yale University bioethicist.
An exodus of volunteers in earlier stages of testing could delay
access to shots that may prove more effective, easier to deliver or
less expensive, said Marc Lipsitch, professor of epidemiology at
Harvard University.
"If we stop a few months in, we're in some sense wasting the
altruistic act of those people who volunteer in the first place,"
argued Mr. Lipsitch. "We get a fraction of the data we could get if
we could continue it."
Frederick Feit, who volunteered for Pfizer's vaccine trial and
thinks he got a placebo, said he would leave the study as soon as
he can to get the shot because that was his purpose for enrolling.
"It was never altruistic," said Dr. Feit, a 72-year-old
cardiologist at NYU Langone Health.
About 48 Covid-19 vaccines are being tested in people, according
to the World Health Organization, studies that researchers designed
to assess whether the shots safely protect against the disease. To
make that assessment, volunteers are randomly given either the
experimental vaccine or a placebo. Neither the volunteers nor
researchers know who got which.
After a sufficient number of subjects develop Covid-19,
researchers take a look to see how many of the volunteers were on a
placebo. The vaccine provides protection if fewer vaccinated
subjects fell sick.
Given the urgent need, researchers will assess whether shots
work safely weeks after study subjects get inoculated. Pfizer and
its partner BioNTech SE, as well as Moderna, have said their
vaccines were roughly 95% effective and appeared safe. AstraZeneca
PLC said its shot was 62% to 90% effective, depending on
dosage.
Data for vaccine candidates from Johnson & Johnson and
Novavax Inc. are expected in the coming months.
The rapid readouts compared with the longer testing schedules of
most vaccine development in the past should help accelerate the
approval and availability of the inoculations. It will also,
however, make it more difficult to answer important questions,
including whether there are any long-term side effects and the
duration of protection provided by the shots.
Better data also would help doctors and health authorities allay
the fears of some Americans reluctant to take a Covid-19 vaccine,
researchers say.
As companies release data from their late-stage vaccine trials
and the leading candidates move closer to authorization, some study
subjects have taken antibody tests to see whether they got the
vaccine or placebo. If it appears they took a placebo, some
volunteers have begun clamoring for access to a vaccine.
"These companies were smart enough to recruit high-risk people
into their studies. Those are the same people who are going to say
'I'm out of here, I'm going to go get something to protect myself'"
when a vaccine becomes available, said Amy Warren, 48, a nurse
practitioner in Kansas City, Mo., who is in a Moderna trial and
signed the letter volunteers sent to the FDA.
Johnson & Johnson last month sought guidance on the matter
from the committee of independent experts advising the FDA on
vaccines. J&J expressed concern that clearance of the first
vaccine would compromise other companies' ability to recruit
volunteers for their own studies, and make it harder to keep
volunteers enrolled if they are eligible for the first vaccine.
Pfizer, however, wrote in its own comment letter that it has an
ethical responsibility to inform trial volunteers if a vaccine was
approved and to provide it to placebo recipients. The company told
study subjects this month that it is exploring how to give the
vaccine to these volunteers but needs regulators to approve.
Marion Gruber, director of the FDA's Center for Biologics
Evaluation and Research, said during a recent panel appearance that
the agency is talking with vaccine makers about how to achieve the
goal of data collection while also making vaccines available to
those who need them most.
Meanwhile, in the U.K., regulators sent a bulletin to Covid-19
vaccine study subjects there this month saying they would be
contacted if a vaccine is cleared, and told if they got the placebo
and are eligible to receive the real shot.
--Jared S. Hopkins and Jenny Strasburg contributed to this
article.
Write to Rolfe Winkler at rolfe.winkler@wsj.com
(END) Dow Jones Newswires
November 27, 2020 09:14 ET (14:14 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
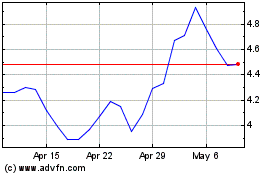
Novavax (NASDAQ:NVAX)
Historical Stock Chart
From Mar 2024 to Apr 2024
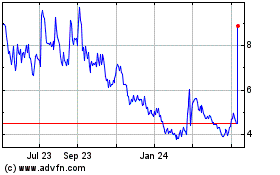
Novavax (NASDAQ:NVAX)
Historical Stock Chart
From Apr 2023 to Apr 2024