Bristol Myers Squibb (NYSE: BMY) today announced the Phase 3
RELATIVITY-098 trial evaluating Opdualag™ (nivolumab and
relatlimab-rmbw) for the adjuvant treatment of patients with
completely resected stage III-IV melanoma did not meet its primary
endpoint of recurrence-free survival (RFS). The safety profile of
Opdualag observed in this analysis was consistent with the known
profiles of nivolumab and relatlimab.
“We are disappointed in the outcome of the RELATIVITY-098 trial
and that LAG-3 inhibition in the adjuvant setting did not lead to
the same improved efficacy outcomes seen in advanced melanoma,”
said Jeffrey Walch, M.D., Ph.D., vice president, Opdualag global
program lead, Bristol Myers Squibb. “Patients whose tumors are
completely resected before treatment may not have sufficient
antitumor T cells in place for Opdualag to have its maximal effect.
However, Opdualag remains a standard of care in the first-line
treatment of unresectable or metastatic melanoma, and we continue
to explore its potential across tumor types, including in non-small
cell lung cancer.”
In adjuvant melanoma, Opdivo® (nivolumab) remains a standard of
care for adult and pediatric patients 12 years and older with
completely resected Stage IIB, Stage IIC, Stage III, or Stage IV
melanoma. Moreover, Opdivo QvantigTM (nivolumab +
hyaluronidase-nvhy), was recently approved in the U.S. as a
subcutaneous option for the adjuvant treatment of adult patients
with completely resected Stage IIB, Stage IIC, Stage III, or Stage
IV melanoma.
BMS thanks the patients, families and investigators for their
contributions to this important clinical trial.
About RELATIVITY-098
RELATIVITY-098 is a randomized Phase 3, double-blind study
evaluating adjuvant immunotherapy with Opdualag, the fixed-dose
combination of nivolumab and relatlimab, compared to Opdivo
monotherapy after complete resection of stage III-IV melanoma.
The primary endpoint of the trial is recurrence-free survival
(RFS). Secondary endpoints include overall survival (OS), distant
metastasis-free survival (DMFS), and safety.
About Opdualag Opdualag
(nivolumab and relatlimab-rmbw) is a first-in-class, fixed-dose,
dual immunotherapy combination of the programmed death-1 (PD-1)
inhibitor nivolumab and the lymphocyte activation gene 3 (LAG-3)
blocking antibody relatlimab.
With its approval by the FDA in 2022, Opdualag became the first
LAG-3-blocking antibody containing combination to receive
regulatory approval anywhere in the world.
About LAG-3
Lymphocyte-activation gene 3 (LAG-3) is a molecule found on the
surface of several immune cell types including CD4+ and CD8+ T
cells, regulatory T cells (Tregs), and natural killer (NK) cells.
LAG-3 inhibits the function of T cells and reduces the activation
and growth of the cell on which it is found. This T-cell
dysfunction allows tumors to avoid attack from the immune system
and grow unchecked.
Preclinical studies indicate that inhibition of LAG-3 may
promote an anti-tumor response. Targeting both LAG-3 and PD-1 in
combination may be a key strategy to help restore T cell activity,
improving anti-tumor response in certain cancers that is greater
than the effects of PD-1 monotherapy.
Bristol Myers Squibb is evaluating relatlimab in clinical trials
in combination with other agents in a variety of tumor types.
About Melanoma Melanoma is a
form of skin cancer characterized by the uncontrolled growth of
pigment-producing cells (melanocytes) located in the skin.
Metastatic melanoma is the deadliest form of the disease and occurs
when cancer spreads beyond the surface of the skin to other organs.
Globally, the World Health Organization estimates that by 2035,
melanoma incidence will reach 424,102, with 94,308 related deaths.
Melanomas can be mostly treatable when caught in very early stages;
however, survival rates can decrease as the disease progresses.
INDICATION
Opdualag™ (nivolumab and relatlimab-rmbw) is indicated for the
treatment of adult and pediatric patients 12 years of age or older
with unresectable or metastatic melanoma.
IMPORTANT SAFETY
INFORMATION
Severe and Fatal Immune-Mediated Adverse Reactions
Immune-mediated adverse reactions (IMARs) listed herein may not
include all possible severe and fatal immune-mediated adverse
reactions.
IMARs which may be severe or fatal, can occur in any organ
system or tissue. IMARs can occur at any time after starting
treatment with a LAG-3 and PD-1/PD-L1 blocking antibodies. While
IMARs usually manifest during treatment, they can also occur after
discontinuation of Opdualag. Early identification and management of
IMARs are essential to ensure safe use. Monitor patients closely
for symptoms and signs that may be clinical manifestations of
underlying IMARs. Evaluate clinical chemistries including liver
enzymes, creatinine, and thyroid function at baseline and
periodically during treatment. In cases of suspected IMARs,
initiate appropriate workup to exclude alternative etiologies,
including infection. Institute medical management promptly,
including specialty consultation as appropriate.
Withhold or permanently discontinue Opdualag depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information). In general, if Opdualag
requires interruption or discontinuation, administer systemic
corticosteroid therapy (1 to 2 mg/kg/day prednisone or equivalent)
until improvement to Grade 1 or less. Upon improvement to Grade 1
or less, initiate corticosteroid taper and continue to taper over
at least 1 month. Consider administration of other systemic
immunosuppressants in patients whose IMARs are not controlled with
corticosteroid therapy. Toxicity management guidelines for adverse
reactions that do not necessarily require systemic steroids (e.g.,
endocrinopathies and dermatologic reactions) are discussed
below.
Immune-Mediated Pneumonitis
Opdualag can cause immune-mediated pneumonitis, which may be
fatal. In patients treated with other PD- 1/PD-L1 blocking
antibodies, the incidence of pneumonitis is higher in patients who
have received prior thoracic radiation. Immune-mediated pneumonitis
occurred in 3.7% (13/355) of patients receiving Opdualag, including
Grade 3 (0.6%), and Grade 2 (2.3%) adverse reactions. Pneumonitis
led to permanent discontinuation of Opdualag in 0.8% and
withholding of Opdualag in 1.4% of patients.
Immune-Mediated Colitis
Opdualag can cause immune-mediated colitis, defined as requiring
use of corticosteroids and no clear alternate etiology. A common
symptom included in the definition of colitis was diarrhea.
Cytomegalovirus infection/reactivation has been reported in
patients with corticosteroid-refractory immune-mediated colitis. In
cases of corticosteroid-refractory colitis, consider repeating
infectious workup to exclude alternative etiologies.
Immune-mediated diarrhea or colitis occurred in 7% (24/355) of
patients receiving Opdualag, including Grade 3 (1.1%) and Grade 2
(4.5%) adverse reactions. Colitis led to permanent discontinuation
of Opdualag in 2% and withholding of Opdualag in 2.8% of
patients.
Immune-Mediated Hepatitis
Opdualag can cause immune-mediated hepatitis, defined as
requiring the use of corticosteroids and no clear alternate
etiology.
Immune-mediated hepatitis occurred in 6% (20/355) of patients
receiving Opdualag, including Grade 4 (0.6%), Grade 3 (3.4%), and
Grade 2 (1.4%) adverse reactions. Hepatitis led to permanent
discontinuation of Opdualag in 1.7% and withholding of Opdualag in
2.3% of patients.
Immune-Mediated
Endocrinopathies
Opdualag can cause primary or secondary adrenal insufficiency,
hypophysitis, thyroid disorders, and Type 1 diabetes mellitus,
which can be present with diabetic ketoacidosis. Withhold or
permanently discontinue Opdualag depending on severity (please see
section 2 Dosage and Administration in the accompanying Full
Prescribing Information).
For Grade 2 or higher adrenal insufficiency, initiate
symptomatic treatment, including hormone replacement as clinically
indicated. In patients receiving Opdualag, adrenal insufficiency
occurred in 4.2% (15/355) of patients receiving Opdualag, including
Grade 3 (1.4%) and Grade 2 (2.5%) adverse reactions. Adrenal
insufficiency led to permanent discontinuation of Opdualag in 1.1%
and withholding of Opdualag in 0.8% of patients.
Hypophysitis can present with acute symptoms associated with
mass effect such as headache, photophobia, or visual field defects.
Hypophysitis can cause hypopituitarism; initiate hormone
replacement as clinically indicated. Hypophysitis occurred in 2.5%
(9/355) of patients receiving Opdualag, including Grade 3 (0.3%)
and Grade 2 (1.4%) adverse reactions. Hypophysitis led to permanent
discontinuation of Opdualag in 0.3% and withholding of Opdualag in
0.6% of patients.
Thyroiditis can present with or without endocrinopathy.
Hypothyroidism can follow hyperthyroidism; initiate hormone
replacement or medical management as clinically indicated.
Thyroiditis occurred in 2.8% (10/355) of patients receiving
Opdualag, including Grade 2 (1.1%) adverse reactions. Thyroiditis
did not lead to permanent discontinuation of Opdualag. Thyroiditis
led to withholding of Opdualag in 0.3% of patients. Hyperthyroidism
occurred in 6% (22/355) of patients receiving Opdualag, including
Grade 2 (1.4%) adverse reactions.
Hyperthyroidism did not lead to permanent discontinuation of
Opdualag. Hyperthyroidism led to withholding of Opdualag in 0.3% of
patients. Hypothyroidism occurred in 17% (59/355) of patients
receiving Opdualag, including Grade 2 (11%) adverse reactions.
Hypothyroidism led to the permanent discontinuation of Opdualag in
0.3% and withholding of Opdualag in 2.5% of patients.
Monitor patients for hyperglycemia or other signs and symptoms
of diabetes; initiate treatment with insulin as clinically
indicated. Diabetes occurred in 0.3% (1/355) of patients receiving
Opdualag, a Grade 3 (0.3%) adverse reaction, and no cases of
diabetic ketoacidosis. Diabetes did not lead to the permanent
discontinuation or withholding of Opdualag in any patient.
Immune-Mediated Nephritis with Renal
Dysfunction
Opdualag can cause immune-mediated nephritis, which is defined
as requiring use of steroids and no clear etiology. In patients
receiving Opdualag, immune-mediated nephritis and renal dysfunction
occurred in 2% (7/355) of patients, including Grade 3 (1.1%) and
Grade 2 (0.8%) adverse reactions. Immune-mediated nephritis and
renal dysfunction led to permanent discontinuation of Opdualag in
0.8% and withholding of Opdualag in 0.6% of patients.
Withhold or permanently discontinue Opdualag depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
Immune-Mediated Dermatologic Adverse
Reactions
Opdualag can cause immune-mediated rash or dermatitis, defined
as requiring use of steroids and no clear alternate etiology.
Exfoliative dermatitis, including Stevens-Johnson syndrome, toxic
epidermal necrolysis, and Drug Rash with eosinophilia and systemic
symptoms has occurred with PD-1/L-1 blocking antibodies. Topical
emollients and/or topical corticosteroids may be adequate to treat
mild to moderate non-exfoliative rashes.
Withhold or permanently discontinue Opdualag depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
Immune-mediated rash occurred in 9% (33/355) of patients,
including Grade 3 (0.6%) and Grade 2 (3.4%) adverse reactions.
Immune-mediated rash did not lead to permanent discontinuation of
Opdualag. Immune- mediated rash led to withholding of Opdualag in
1.4% of patients.
Immune-Mediated Myocarditis
Opdualag can cause immune-mediated myocarditis, which is defined
as requiring use of steroids and no clear alternate etiology. The
diagnosis of immune-mediated myocarditis requires a high index of
suspicion. Patients with cardiac or cardio-pulmonary symptoms
should be assessed for potential myocarditis. If myocarditis is
suspected, withhold dose, promptly initiate high dose steroids
(prednisone or methylprednisolone 1 to 2 mg/kg/day) and promptly
arrange cardiology consultation with diagnostic workup. If
clinically confirmed, permanently discontinue Opdualag for Grade
2-4 myocarditis.
Myocarditis occurred in 1.7% (6/355) of patients receiving
Opdualag, including Grade 3 (0.6%), and Grade 2 (1.1%) adverse
reactions. Myocarditis led to permanent discontinuation of Opdualag
in 1.7% of patients.
Other Immune-Mediated Adverse
Reactions
The following clinically significant IMARs occurred at an
incidence of <1% (unless otherwise noted) in patients who
received Opdualag or were reported with the use of other PD-1/PD-L1
blocking antibodies. Severe or fatal cases have been reported for
some of these adverse reactions: Cardiac/Vascular: pericarditis,
vasculitis; Nervous System: meningitis, encephalitis, myelitis and
demyelination, myasthenic syndrome/myasthenia gravis (including
exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune
neuropathy; Ocular: uveitis, iritis, and other ocular inflammatory
toxicities can occur. Some cases can be associated with retinal
detachment.
Various grades of visual impairment, including blindness, can
occur. If uveitis occurs in combination with other IMARs, consider
a Vogt-Koyanagi-Harada–like syndrome, as this may require treatment
with systemic steroids to reduce the risk of permanent vision loss;
Gastrointestinal: pancreatitis including increases in serum amylase
and lipase levels, gastritis, duodenitis; Musculoskeletal and
Connective Tissue: myositis/polymyositis, rhabdomyolysis (and
associated sequelae including renal failure), arthritis,
polymyalgia rheumatica; Endocrine: hypoparathyroidism; Other
(Hematologic/Immune): hemolytic anemia, aplastic anemia,
hemophagocytic lymphohistiocytosis, systemic inflammatory response
syndrome, histiocytic necrotizing lymphadenitis (Kikuchi
lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, solid
organ transplant rejection, other transplant (including corneal
graft) rejection.
Infusion-Related Reactions
Opdualag can cause severe infusion-related reactions.
Discontinue Opdualag in patients with severe or life- threatening
infusion-related reactions. Interrupt or slow the rate of infusion
in patients with mild to moderate infusion-related reactions. In
patients who received Opdualag as a 60-minute intravenous infusion,
infusion- related reactions occurred in 7% (23/355) of
patients.
Complications of Allogeneic Hematopoietic Stem Cell
Transplantation (HSCT)
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with a PD-1/PD-L1 receptor blocking
antibody. Transplant- related complications include hyperacute
graft-versus-host disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease after reduced intensity conditioning, and
steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between PD-1/PD-L1 blockade and allogeneic
HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with a PD-1/PD-L1 receptor blocking antibody
prior to or after an allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal studies,
Opdualag can cause fetal harm when administered to a pregnant
woman. Advise pregnant women of the potential risk to a fetus.
Advise females of reproductive potential to use effective
contraception during treatment with Opdualag and for at least 5
months after the last dose of Opdualag.
Lactation
There are no data on the presence of Opdualag in human milk, the
effects on the breastfed child, or the effect on milk production.
Because nivolumab and relatlimab may be excreted in human milk and
because of the potential for serious adverse reactions in a
breastfed child, advise patients not to breastfeed during treatment
with Opdualag and for at least 5 months after the last dose.
Serious Adverse Reactions
In Relativity-047, fatal adverse reactions occurred in 3 (0.8%)
patients who were treated with Opdualag; these included
hemophagocytic lymphohistiocytosis, acute edema of the lung, and
pneumonitis. Serious adverse reactions occurred in 36% of patients
treated with Opdualag. The most frequent serious adverse reactions
reported in ≥1% of patients treated with Opdualag were adrenal
insufficiency (1.4%), anemia (1.4%), colitis (1.4%), pneumonia
(1.4%), acute myocardial infarction (1.1%), back pain (1.1%),
diarrhea (1.1%), myocarditis (1.1%), and pneumonitis (1.1%).
Common Adverse Reactions and Laboratory Abnormalities
The most common adverse reactions reported in ≥20% of the
patients treated with Opdualag were musculoskeletal pain (45%),
fatigue (39%), rash (28%), pruritus (25%), and diarrhea (24%).
The most common laboratory abnormalities that occurred in ≥20%
of patients treated with Opdualag were decreased hemoglobin (37%),
decreased lymphocytes (32%), increased AST (30%), increased ALT
(26%), and decreased sodium (24%).
Please see U.S. Full Prescribing Information for Opdualag.
INDICATIONS
OPDIVO® (nivolumab), as a single agent, is indicated for the
treatment of adult and pediatric patients 12 years and older with
unresectable or metastatic melanoma.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the treatment of adult and pediatric patients 12
years and older with unresectable or metastatic melanoma.
OPDIVO® is indicated for the adjuvant treatment of adult and
pediatric patients 12 years and older with completely resected
Stage IIB, Stage IIC, Stage III, or Stage IV melanoma.
OPDIVO® (nivolumab), in combination with platinum-doublet
chemotherapy, is indicated as neoadjuvant treatment of adult
patients with resectable (tumors ≥4 cm or node positive) non-small
cell lung cancer (NSCLC).
OPDIVO® (nivolumab) in combination with platinum-doublet
chemotherapy, is indicated for neoadjuvant treatment of adult
patients with resectable (tumors ≥4 cm or node positive) non-small
cell lung cancer (NSCLC) and no known epidermal growth factor
receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK)
rearrangements, followed by single-agent OPDIVO® as adjuvant
treatment after surgery.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
metastatic non-small cell lung cancer (NSCLC) whose tumors express
PD-L1 (≥1%) as determined by an FDA-approved test, with no EGFR or
ALK genomic tumor aberrations.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab)
and 2 cycles of platinum-doublet chemotherapy, is indicated for the
first-line treatment of adult patients with metastatic or recurrent
non-small cell lung cancer (NSCLC), with no EGFR or ALK genomic
tumor aberrations.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with metastatic non-small cell lung cancer (NSCLC) with
progression on or after platinum-based chemotherapy. Patients with
EGFR or ALK genomic tumor aberrations should have disease
progression on FDA-approved therapy for these aberrations prior to
receiving OPDIVO.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
unresectable malignant pleural mesothelioma (MPM).
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
intermediate or poor risk advanced renal cell carcinoma (RCC).
OPDIVO® (nivolumab), in combination with cabozantinib, is
indicated for the first-line treatment of adult patients with
advanced renal cell carcinoma (RCC).
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with advanced renal cell carcinoma (RCC) who have received
prior anti-angiogenic therapy.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with classical Hodgkin lymphoma (cHL) that has relapsed or
progressed after autologous hematopoietic stem cell transplantation
(HSCT) and brentuximab vedotin or after 3 or more lines of systemic
therapy that includes autologous HSCT. This indication is approved
under accelerated approval based on overall response rate.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in confirmatory
trials.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with recurrent or metastatic squamous cell carcinoma of
the head and neck (SCCHN) with disease progression on or after
platinum-based therapy.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with locally advanced or metastatic urothelial carcinoma
who have disease progression during or following
platinum-containing chemotherapy or have disease progression within
12 months of neoadjuvant or adjuvant treatment with
platinum-containing chemotherapy.
OPDIVO® (nivolumab), as a single agent, is indicated for the
adjuvant treatment of adult patients with urothelial carcinoma (UC)
who are at high risk of recurrence after undergoing radical
resection of UC.
OPDIVO® (nivolumab), in combination with cisplatin and
gemcitabine, is indicated as first-line treatment for adult
patients with unresectable or metastatic urothelial carcinoma.
OPDIVO® (nivolumab), as a single agent, is indicated for the
treatment of adult and pediatric (12 years and older) patients with
microsatellite instability-high (MSI-H) or mismatch repair
deficient (dMMR) metastatic colorectal cancer (CRC) that has
progressed following treatment with a fluoropyrimidine,
oxaliplatin, and irinotecan. This indication is approved under
accelerated approval based on overall response rate and duration of
response. Continued approval for this indication may be contingent
upon verification and description of clinical benefit in
confirmatory trials.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the treatment of adult and pediatric patients 12
years and older with microsatellite instability-high (MSI-H) or
mismatch repair deficient (dMMR) metastatic colorectal cancer (CRC)
that has progressed following treatment with a fluoropyrimidine,
oxaliplatin, and irinotecan. This indication is approved under
accelerated approval based on overall response rate and duration of
response. Continued approval for this indication may be contingent
upon verification and description of clinical benefit in
confirmatory trials.
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the treatment of adult patients with
hepatocellular carcinoma (HCC) who have been previously treated
with sorafenib. This indication is approved under accelerated
approval based on overall response rate and duration of response.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in the
confirmatory trials.
OPDIVO® (nivolumab) is indicated for the treatment of adult
patients with unresectable advanced, recurrent or metastatic
esophageal squamous cell carcinoma (ESCC) after prior
fluoropyrimidine- and platinum-based chemotherapy.
OPDIVO® (nivolumab) is indicated for the adjuvant treatment of
completely resected esophageal or gastroesophageal junction cancer
with residual pathologic disease in adult patients who have
received neoadjuvant chemoradiotherapy (CRT).
OPDIVO® (nivolumab), in combination with fluoropyrimidine- and
platinum-containing chemotherapy, is indicated for the first-line
treatment of adult patients with unresectable advanced or
metastatic esophageal squamous cell carcinoma (ESCC).
OPDIVO® (nivolumab), in combination with YERVOY® (ipilimumab),
is indicated for the first-line treatment of adult patients with
unresectable advanced or metastatic esophageal squamous cell
carcinoma (ESCC).
OPDIVO® (nivolumab), in combination with fluoropyrimidine- and
platinum-containing chemotherapy, is indicated for the treatment of
adult patients with advanced or metastatic gastric cancer,
gastroesophageal junction cancer, and esophageal
adenocarcinoma.
IMPORTANT SAFETY INFORMATION
Severe and Fatal Immune-Mediated Adverse Reactions
Immune-mediated adverse reactions listed herein may not include
all possible severe and fatal immune- mediated adverse
reactions.
Immune-mediated adverse reactions, which may be severe or fatal,
can occur in any organ system or tissue. While immune-mediated
adverse reactions usually manifest during treatment, they can also
occur after discontinuation of OPDIVO or YERVOY. Early
identification and management are essential to ensure safe use of
OPDIVO and YERVOY. Monitor for signs and symptoms that may be
clinical manifestations of underlying immune-mediated adverse
reactions. Evaluate clinical chemistries including liver enzymes,
creatinine, adrenocorticotropic hormone (ACTH) level, and thyroid
function at baseline and periodically during treatment with OPDIVO
and before each dose of YERVOY. In cases of suspected
immune-mediated adverse reactions, initiate appropriate workup to
exclude alternative etiologies, including infection. Institute
medical management promptly, including specialty consultation as
appropriate.
Withhold or permanently discontinue OPDIVO and YERVOY depending
on severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information). In general, if OPDIVO
or YERVOY interruption or discontinuation is required, administer
systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or
equivalent) until improvement to Grade 1 or less. Upon improvement
to Grade 1 or less, initiate corticosteroid taper and continue to
taper over at least 1 month. Consider administration of other
systemic immunosuppressants in patients whose immune-mediated
adverse reactions are not controlled with corticosteroid therapy.
Toxicity management guidelines for adverse reactions that do not
necessarily require systemic steroids (e.g., endocrinopathies and
dermatologic reactions) are discussed below.
Immune-Mediated Pneumonitis
OPDIVO and YERVOY can cause immune-mediated pneumonitis. The
incidence of pneumonitis is higher in patients who have received
prior thoracic radiation. In patients receiving OPDIVO monotherapy,
immune- mediated pneumonitis occurred in 3.1% (61/1994) of
patients, including Grade 4 (<0.1%), Grade 3 (0.9%), and Grade 2
(2.1%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg
every 3 weeks, immune- mediated pneumonitis occurred in 7% (31/456)
of patients, including Grade 4 (0.2%), Grade 3 (2.0%), and Grade 2
(4.4%). In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg
every 3 weeks, immune- mediated pneumonitis occurred in 3.9%
(26/666) of patients, including Grade 3 (1.4%) and Grade 2 (2.6%).
In NSCLC patients receiving OPDIVO 3 mg/kg every 2 weeks with
YERVOY 1 mg/kg every 6 weeks, immune- mediated pneumonitis occurred
in 9% (50/576) of patients, including Grade 4 (0.5%), Grade 3
(3.5%), and Grade 2 (4.0%). Four patients (0.7%) died due to
pneumonitis.
Immune-Mediated Colitis
OPDIVO and YERVOY can cause immune-mediated colitis, which may
be fatal. A common symptom included in the definition of colitis
was diarrhea. Cytomegalovirus (CMV) infection/reactivation has been
reported in patients with corticosteroid-refractory immune-mediated
colitis. In cases of corticosteroid-refractory colitis, consider
repeating infectious workup to exclude alternative etiologies. In
patients receiving OPDIVO monotherapy, immune-mediated colitis
occurred in 2.9% (58/1994) of patients, including Grade 3 (1.7%)
and Grade 2 (1%). In patients receiving OPDIVO 1 mg/kg with YERVOY
3 mg/kg every 3 weeks, immune-mediated colitis occurred in 25%
(115/456) of patients, including Grade 4 (0.4%), Grade 3 (14%) and
Grade 2 (8%). In patients receiving OPDIVO 3 mg/kg with YERVOY 1
mg/kg every 3 weeks, immune-mediated colitis occurred in 9%
(60/666) of patients, including Grade 3 (4.4%) and Grade 2
(3.7%).
Immune-Mediated Hepatitis and
Hepatotoxicity
OPDIVO and YERVOY can cause immune-mediated hepatitis. In
patients receiving OPDIVO monotherapy, immune-mediated hepatitis
occurred in 1.8% (35/1994) of patients, including Grade 4 (0.2%),
Grade 3 (1.3%), and Grade 2 (0.4%). In patients receiving OPDIVO 1
mg/kg with YERVOY 3 mg/kg every 3 weeks, immune- mediated hepatitis
occurred in 15% (70/456) of patients, including Grade 4 (2.4%),
Grade 3 (11%), and Grade 2 (1.8%). In patients receiving OPDIVO 3
mg/kg with YERVOY 1 mg/kg every 3 weeks, immune-mediated hepatitis
occurred in 7% (48/666) of patients, including Grade 4 (1.2%),
Grade 3 (4.9%), and Grade 2 (0.4%).
OPDIVO in combination with cabozantinib can cause hepatic
toxicity with higher frequencies of Grade 3 and 4 ALT and AST
elevations compared to OPDIVO alone. Consider more frequent
monitoring of liver enzymes as compared to when the drugs are
administered as single agents. In patients receiving OPDIVO and
cabozantinib, Grades 3 and 4 increased ALT or AST were seen in 11%
of patients.
Immune-Mediated
Endocrinopathies
OPDIVO and YERVOY can cause primary or secondary adrenal
insufficiency, immune-mediated hypophysitis, immune-mediated
thyroid disorders, and Type 1 diabetes mellitus, which can present
with diabetic ketoacidosis. Withhold OPDIVO and YERVOY depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information). For Grade 2 or higher
adrenal insufficiency, initiate symptomatic treatment, including
hormone replacement as clinically indicated. Hypophysitis can
present with acute symptoms associated with mass effect such as
headache, photophobia, or visual field defects. Hypophysitis can
cause hypopituitarism; initiate hormone replacement as clinically
indicated. Thyroiditis can present with or without endocrinopathy.
Hypothyroidism can follow hyperthyroidism; initiate hormone
replacement or medical management as clinically indicated. Monitor
patients for hyperglycemia or other signs and symptoms of diabetes;
initiate treatment with insulin as clinically indicated.
In patients receiving OPDIVO monotherapy, adrenal insufficiency
occurred in 1% (20/1994), including Grade 3 (0.4%) and Grade 2
(0.6%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg
every 3 weeks, adrenal insufficiency occurred in 8% (35/456),
including Grade 4 (0.2%), Grade 3 (2.4%), and Grade 2 (4.2%). In
patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, adrenal insufficiency occurred in 7% (48/666) of patients,
including Grade 4 (0.3%), Grade 3 (2.5%), and Grade 2 (4.1%). In
patients receiving OPDIVO and cabozantinib, adrenal insufficiency
occurred in 4.7% (15/320) of patients, including Grade 3 (2.2%) and
Grade 2 (1.9%).
In patients receiving OPDIVO monotherapy, hypophysitis occurred
in 0.6% (12/1994) of patients, including Grade 3 (0.2%) and Grade 2
(0.3%).
In patients receiving OPDIVO 1 mg/kg with YERVOY 3 mg/kg every 3
weeks, hypophysitis occurred in 9% (42/456), including Grade 3
(2.4%) and Grade 2 (6%). In patients receiving OPDIVO 3 mg/kg with
YERVOY 1 mg/kg every 3 weeks, hypophysitis occurred in 4.4%
(29/666) of patients, including Grade 4 (0.3%), Grade 3 (2.4%), and
Grade 2 (0.9%).
In patients receiving OPDIVO monotherapy, thyroiditis occurred
in 0.6% (12/1994) of patients, including Grade 2 (0.2%). In
patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, thyroiditis occurred in 2.7% (22/666) of patients, including
Grade 3 (4.5%) and Grade 2 (2.2%).
In patients receiving OPDIVO monotherapy, hyperthyroidism
occurred in 2.7% (54/1994) of patients, including Grade 3
(<0.1%) and Grade 2 (1.2%). In patients receiving OPDIVO 1 mg/kg
with YERVOY 3 mg/kg every 3 weeks, hyperthyroidism occurred in 9%
(42/456) of patients, including Grade 3 (0.9%) and Grade 2 (4.2%).
In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, hyperthyroidism occurred in 12% (80/666) of patients,
including Grade 3 (0.6%) and Grade 2 (4.5%).
In patients receiving OPDIVO monotherapy, hypothyroidism
occurred in 8% (163/1994) of patients, including Grade 3 (0.2%) and
Grade 2 (4.8%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3
mg/kg every 3 weeks, hypothyroidism occurred in 20% (91/456) of
patients, including Grade 3 (0.4%) and Grade 2 (11%). In patients
receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3 weeks,
hypothyroidism occurred in 18% (122/666) of patients, including
Grade 3 (0.6%) and Grade 2 (11%).
In patients receiving OPDIVO monotherapy, diabetes occurred in
0.9% (17/1994) of patients, including Grade 3 (0.4%) and Grade 2
(0.3%), and 2 cases of diabetic ketoacidosis. In patients receiving
OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3 weeks, diabetes occurred
in 2.7% (15/666) of patients, including Grade 4 (0.6%), Grade 3
(0.3%), and Grade 2 (0.9%).
Immune-Mediated Nephritis with Renal
Dysfunction
OPDIVO and YERVOY can cause immune-mediated nephritis. In
patients receiving OPDIVO monotherapy, immune-mediated nephritis
and renal dysfunction occurred in 1.2% (23/1994) of patients,
including Grade 4 (<0.1%), Grade 3 (0.5%), and Grade 2 (0.6%).
In patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, immune-mediated nephritis with renal dysfunction occurred in
4.1% (27/666) of patients, including Grade 4 (0.6%), Grade 3
(1.1%), and Grade 2 (2.2%).
Immune-Mediated Dermatologic Adverse
Reactions
OPDIVO can cause immune-mediated rash or dermatitis. Exfoliative
dermatitis, including Stevens-Johnson syndrome (SJS), toxic
epidermal necrolysis (TEN), and drug rash with eosinophilia and
systemic symptoms (DRESS) has occurred with PD-1/PD-L1 blocking
antibodies. Topical emollients and/or topical corticosteroids may
be adequate to treat mild to moderate nonexfoliative rashes.
YERVOY can cause immune-mediated rash or dermatitis, including
bullous and exfoliative dermatitis, SJS, TEN, and DRESS. Topical
emollients and/or topical corticosteroids may be adequate to treat
mild to moderate non-bullous/exfoliative rashes.
Withhold or permanently discontinue OPDIVO and YERVOY depending
on severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
In patients receiving OPDIVO monotherapy, immune-mediated rash
occurred in 9% (171/1994) of patients, including Grade 3 (1.1%) and
Grade 2 (2.2%). In patients receiving OPDIVO 1 mg/kg with YERVOY 3
mg/kg every 3 weeks, immune-mediated rash occurred in 28% (127/456)
of patients, including Grade 3 (4.8%) and Grade 2 (10%). In
patients receiving OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3
weeks, immune-mediated rash occurred in 16% (108/666) of patients,
including Grade 3 (3.5%) and Grade 2 (4.2%).
Other Immune-Mediated Adverse
Reactions
The following clinically significant immune-mediated adverse
reactions occurred at an incidence of <1% (unless otherwise
noted) in patients who received OPDIVO monotherapy or OPDIVO in
combination with YERVOY or were reported with the use of other
PD-1/PD-L1 blocking antibodies. Severe or fatal cases have been
reported for some of these adverse reactions: cardiac/vascular:
myocarditis, pericarditis, vasculitis; nervous system: meningitis,
encephalitis, myelitis and demyelination, myasthenic
syndrome/myasthenia gravis (including exacerbation), Guillain-Barré
syndrome, nerve paresis, autoimmune neuropathy; ocular: uveitis,
iritis, and other ocular inflammatory toxicities can occur;
gastrointestinal: pancreatitis to include increases in serum
amylase and lipase levels, gastritis, duodenitis; musculoskeletal
and connective tissue: myositis/polymyositis, rhabdomyolysis, and
associated sequelae including renal failure, arthritis, polymyalgia
rheumatica; endocrine: hypoparathyroidism; other
(hematologic/immune): hemolytic anemia, aplastic anemia,
hemophagocytic lymphohistiocytosis (HLH), systemic inflammatory
response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi
lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, solid
organ transplant rejection, other transplant (including corneal
graft) rejection.
In addition to the immune-mediated adverse reactions listed
above, across clinical trials of YERVOY monotherapy or in
combination with OPDIVO, the following clinically significant
immune-mediated adverse reactions, some with fatal outcome,
occurred in <1% of patients unless otherwise specified: nervous
system: autoimmune neuropathy (2%), myasthenic syndrome/myasthenia
gravis, motor dysfunction; cardiovascular: angiopathy, temporal
arteritis; ocular: blepharitis, episcleritis, orbital myositis,
scleritis; gastrointestinal: pancreatitis (1.3%); other
(hematologic/immune): conjunctivitis, cytopenias (2.5%),
eosinophilia (2.1%), erythema multiforme, hypersensitivity
vasculitis, neurosensory hypoacusis, psoriasis.
Some ocular IMAR cases can be associated with retinal
detachment. Various grades of visual impairment, including
blindness, can occur. If uveitis occurs in combination with other
immune-mediated adverse reactions, consider a
Vogt-Koyanagi-Harada–like syndrome, which has been observed in
patients receiving OPDIVO and YERVOY, as this may require treatment
with systemic corticosteroids to reduce the risk of permanent
vision loss.
Infusion-Related Reactions
OPDIVO and YERVOY can cause severe infusion-related reactions.
Discontinue OPDIVO and YERVOY in patients with severe (Grade 3) or
life-threatening (Grade 4) infusion-related reactions. Interrupt or
slow the rate of infusion in patients with mild (Grade 1) or
moderate (Grade 2) infusion-related reactions. In patients
receiving OPDIVO monotherapy as a 60-minute infusion,
infusion-related reactions occurred in 6.4% (127/1994) of patients.
In a separate trial in which patients received OPDIVO monotherapy
as a 60-minute infusion or a 30- minute infusion, infusion-related
reactions occurred in 2.2% (8/368) and 2.7% (10/369) of patients,
respectively. Additionally, 0.5% (2/368) and 1.4% (5/369) of
patients, respectively, experienced adverse reactions within 48
hours of infusion that led to dose delay, permanent discontinuation
or withholding of OPDIVO. In melanoma patients receiving OPDIVO 1
mg/kg with YERVOY 3 mg/kg every 3 weeks, infusion-related reactions
occurred in 2.5% (10/407) of patients. In RCC patients receiving
OPDIVO 3 mg/kg with YERVOY 1 mg/kg every 3 weeks, infusion-related
reactions occurred in 5.1% (28/547) of patients. In MPM patients
receiving OPDIVO 3 mg/kg every 2 weeks with YERVOY 1 mg/kg every 6
weeks, infusion-related reactions occurred in 12% (37/300) of
patients.
Complications of Allogeneic Hematopoietic Stem Cell
Transplantation
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with OPDIVO or YERVOY.
Transplant-related complications include hyperacute
graft-versus-host-disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease (VOD) after reduced intensity conditioning,
and steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between OPDIVO or YERVOY and allogeneic
HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with OPDIVO and YERVOY prior to or after an
allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action and findings from animal
studies, OPDIVO and YERVOY can cause fetal harm when administered
to a pregnant woman. The effects of YERVOY are likely to be greater
during the second and third trimesters of pregnancy. Advise
pregnant women of the potential risk to a fetus. Advise females of
reproductive potential to use effective contraception during
treatment with OPDIVO and YERVOY and for at least 5 months after
the last dose.
Increased Mortality in Patients with Multiple Myeloma when
OPDIVO is Added to a Thalidomide Analogue and Dexamethasone
In randomized clinical trials in patients with multiple myeloma,
the addition of OPDIVO to a thalidomide analogue plus dexamethasone
resulted in increased mortality. Treatment of patients with
multiple myeloma with a PD-1 or PD-L1 blocking antibody in
combination with a thalidomide analogue plus dexamethasone is not
recommended outside of controlled clinical trials.
Lactation
There are no data on the presence of OPDIVO or YERVOY in human
milk, the effects on the breastfed child, or the effects on milk
production. Because of the potential for serious adverse reactions
in breastfed children, advise women not to breastfeed during
treatment and for 5 months after the last dose.
Serious Adverse Reactions
In Checkmate 037, serious adverse reactions occurred in 41% of
patients receiving OPDIVO (n=268). Grade 3 and 4 adverse reactions
occurred in 42% of patients receiving OPDIVO. The most frequent
Grade 3 and 4 adverse drug reactions reported in 2% to <5% of
patients receiving OPDIVO were abdominal pain, hyponatremia,
increased aspartate aminotransferase, and increased lipase. In
Checkmate 066, serious adverse reactions occurred in 36% of
patients receiving OPDIVO (n=206). Grade 3 and 4 adverse reactions
occurred in 41% of patients receiving OPDIVO. The most frequent
Grade 3 and 4 adverse reactions reported in ≥2% of patients
receiving OPDIVO were gamma-glutamyltransferase increase (3.9%) and
diarrhea (3.4%). In Checkmate 067, serious adverse reactions (74%
and 44%), adverse reactions leading to permanent discontinuation
(47% and 18%) or to dosing delays (58% and 36%), and Grade 3 or 4
adverse reactions (72% and 51%) all occurred more frequently in the
OPDIVO plus YERVOY arm (n=313) relative to the OPDIVO arm (n=313).
The most frequent (≥10%) serious adverse reactions in the OPDIVO
plus YERVOY arm and the OPDIVO arm, respectively, were diarrhea
(13% and 2.2%), colitis (10% and 1.9%), and pyrexia (10% and 1.0%).
In Checkmate 238, serious adverse reactions occurred in 18% of
patients receiving OPDIVO (n=452). Grade 3 or 4 adverse reactions
occurred in 25% of OPDIVO-treated patients (n=452). The most
frequent Grade 3 and 4 adverse reactions reported in ≥2% of
OPDIVO-treated patients were diarrhea and increased lipase and
amylase. In Checkmate 816, serious adverse reactions occurred in
30% of patients (n=176) who were treated with OPDIVO in combination
with platinum-doublet chemotherapy. Serious adverse reactions in
>2% included pneumonia and vomiting. No fatal adverse reactions
occurred in patients who received OPDIVO in combination with
platinum-doublet chemotherapy. In Checkmate 77T, serious adverse
reactions occurred in 21% of patients who received OPDIVO in
combination with platinum-doublet chemotherapy as neoadjuvant
treatment (n=228). The most frequent (≥2%) serious adverse
reactions was pneumonia. Fatal adverse reactions occurred in 2.2%
of patients, due to cerebrovascular accident, COVID-19 infection,
hemoptysis, pneumonia, and pneumonitis (0.4% each). In the adjuvant
phase of Checkmate 77T, 22% of patients experienced serious adverse
reactions (n=142). The most frequent serious adverse reaction was
pneumonitis/ILD (2.8%). One fatal adverse reaction due to COVID-19
occurred. In Checkmate 227, serious adverse reactions occurred in
58% of patients (n=576). The most frequent (≥2%) serious adverse
reactions were pneumonia, diarrhea/colitis, pneumonitis, hepatitis,
pulmonary embolism, adrenal insufficiency, and hypophysitis. Fatal
adverse reactions occurred in 1.7% of patients; these included
events of pneumonitis (4 patients), myocarditis, acute kidney
injury, shock, hyperglycemia, multi-system organ failure, and renal
failure. In Checkmate 9LA, serious adverse reactions occurred in
57% of patients (n=358). The most frequent (>2%) serious adverse
reactions were pneumonia, diarrhea, febrile neutropenia, anemia,
acute kidney injury, musculoskeletal pain, dyspnea, pneumonitis,
and respiratory failure. Fatal adverse reactions occurred in 7 (2%)
patients, and included hepatic toxicity, acute renal failure,
sepsis, pneumonitis, diarrhea with hypokalemia, and massive
hemoptysis in the setting of thrombocytopenia. In Checkmate 017 and
057, serious adverse reactions occurred in 46% of patients
receiving OPDIVO (n=418). The most frequent serious adverse
reactions reported in ≥2% of patients receiving OPDIVO were
pneumonia, pulmonary embolism, dyspnea, pyrexia, pleural effusion,
pneumonitis, and respiratory failure. In Checkmate 057, fatal
adverse reactions occurred; these included events of infection (7
patients, including one case of Pneumocystis jirovecii pneumonia),
pulmonary embolism (4 patients), and limbic encephalitis (1
patient). In Checkmate 743, serious adverse reactions occurred in
54% of patients receiving OPDIVO plus YERVOY. The most frequent
serious adverse reactions reported in ≥2% of patients were
pneumonia, pyrexia, diarrhea, pneumonitis, pleural effusion,
dyspnea, acute kidney injury, infusion-related reaction,
musculoskeletal pain, and pulmonary embolism. Fatal adverse
reactions occurred in 4 (1.3%) patients and included pneumonitis,
acute heart failure, sepsis, and encephalitis. In Checkmate 214,
serious adverse reactions occurred in 59% of patients receiving
OPDIVO plus YERVOY (n=547). The most frequent serious adverse
reactions reported in ≥2% of patients were diarrhea, pyrexia,
pneumonia, pneumonitis, hypophysitis, acute kidney injury, dyspnea,
adrenal insufficiency, and colitis. In Checkmate 9ER, serious
adverse reactions occurred in 48% of patients receiving OPDIVO and
cabozantinib (n=320). The most frequent serious adverse reactions
reported in ≥2% of patients were diarrhea, pneumonia, pneumonitis,
pulmonary embolism, urinary tract infection, and hyponatremia.
Fatal intestinal perforations occurred in 3 (0.9%) patients. In
Checkmate 025, serious adverse reactions occurred in 47% of
patients receiving OPDIVO (n=406). The most frequent serious
adverse reactions reported in ≥2% of patients were acute kidney
injury, pleural effusion, pneumonia, diarrhea, and hypercalcemia.
In Checkmate 141, serious adverse reactions occurred in 49% of
patients receiving OPDIVO (n=236). The most frequent serious
adverse reactions reported in ≥2% of patients receiving OPDIVO were
pneumonia, dyspnea, respiratory failure, respiratory tract
infection, and sepsis. In Checkmate 275, serious adverse reactions
occurred in 54% of patients receiving OPDIVO (n=270). The most
frequent serious adverse reactions reported in ≥2% of patients
receiving OPDIVO were urinary tract infection, sepsis, diarrhea,
small intestine obstruction, and general physical health
deterioration. In Checkmate 274, serious adverse reactions occurred
in 30% of patients receiving OPDIVO (n=351). The most frequent
serious adverse reaction reported in ≥2% of patients receiving
OPDIVO was urinary tract infection. Fatal adverse reactions
occurred in 1% of patients; these included events of pneumonitis
(0.6%). In Checkmate 901, serious adverse reactions occurred in 48%
of patients receiving OPDIVO in combination with chemotherapy. The
most frequent serious adverse reactions reporting in ≥2% of
patients who received OPDIVO with chemotherapy were urinary tract
infection (4.9%), acute kidney injury (4.3%), anemia (3%),
pulmonary embolism (2.6%), sepsis (2.3%), and platelet count
decreased (2.3%). Fatal adverse reactions occurred in 3.6% of
patients who received OPDIVO in combination with chemotherapy;
these included sepsis (1%). OPDIVO and/or chemotherapy were
discontinued in 30% of patients and were delayed in 67% of patients
for an adverse reaction. In Attraction-3, serious adverse reactions
occurred in 38% of patients receiving OPDIVO (n=209). Serious
adverse reactions reported in ≥2% of patients who received OPDIVO
were pneumonia, esophageal fistula, interstitial lung disease, and
pyrexia. The following fatal adverse reactions occurred in patients
who received OPDIVO: interstitial lung disease or pneumonitis
(1.4%), pneumonia (1.0%), septic shock (0.5%), esophageal fistula
(0.5%), gastrointestinal hemorrhage (0.5%), pulmonary embolism
(0.5%), and sudden death (0.5%). In Checkmate 577, serious adverse
reactions occurred in 33% of patients receiving OPDIVO (n=532). A
serious adverse reaction reported in ≥2% of patients who received
OPDIVO was pneumonitis. A fatal reaction of myocardial infarction
occurred in one patient who received OPDIVO. In Checkmate 648,
serious adverse reactions occurred in 62% of patients receiving
OPDIVO in combination with chemotherapy (n=310). The most frequent
serious adverse reactions reported in ≥2% of patients who received
OPDIVO with chemotherapy were pneumonia (11%), dysphagia (7%),
esophageal stenosis (2.9%), acute kidney injury (2.9%), and pyrexia
(2.3%). Fatal adverse reactions occurred in 5 (1.6%) patients who
received OPDIVO in combination with chemotherapy; these included
pneumonitis, pneumatosis intestinalis, pneumonia, and acute kidney
injury. In Checkmate 648, serious adverse reactions occurred in 69%
of patients receiving OPDIVO in combination with YERVOY (n=322).
The most frequent serious adverse reactions reported in ≥2% who
received OPDIVO in combination with YERVOY were pneumonia (10%),
pyrexia (4.3%), pneumonitis (4.0%), aspiration pneumonia (3.7%),
dysphagia (3.7%), hepatic function abnormal (2.8%), decreased
appetite (2.8%), adrenal insufficiency (2.5%), and dehydration
(2.5%). Fatal adverse reactions occurred in 5 (1.6%) patients who
received OPDIVO in combination with YERVOY; these included
pneumonitis, interstitial lung disease, pulmonary embolism, and
acute respiratory distress syndrome. In Checkmate 649, serious
adverse reactions occurred in 52% of patients treated with OPDIVO
in combination with chemotherapy (n=782). The most frequent serious
adverse reactions reported in ≥2% of patients treated with OPDIVO
in combination with chemotherapy were vomiting (3.7%), pneumonia
(3.6%), anemia (3.6%), pyrexia (2.8%), diarrhea (2.7%), febrile
neutropenia (2.6%), and pneumonitis (2.4%). Fatal adverse reactions
occurred in 16 (2.0%) patients who were treated with OPDIVO in
combination with chemotherapy; these included pneumonitis (4
patients), febrile neutropenia (2 patients), stroke (2 patients),
gastrointestinal toxicity, intestinal mucositis, septic shock,
pneumonia, infection, gastrointestinal bleeding, mesenteric vessel
thrombosis, and disseminated intravascular coagulation. In
Checkmate 76K, serious adverse reactions occurred in 18% of
patients receiving OPDIVO (n=524). Adverse reactions which resulted
in permanent discontinuation of OPDIVO in >1% of patients
included arthralgia (1.7%), rash (1.7%), and diarrhea (1.1%). A
fatal adverse reaction occurred in 1 (0.2%) patient (heart failure
and acute kidney injury). The most frequent Grade 3-4 lab
abnormalities reported in ≥1% of OPDIVO-treated patients were
increased lipase (2.9%), increased AST (2.2%), increased ALT
(2.1%), lymphopenia (1.1%), and decreased potassium (1.0%).
Common Adverse Reactions
In Checkmate 037, the most common adverse reaction (≥20%)
reported with OPDIVO (n=268) was rash (21%). In Checkmate 066, the
most common adverse reactions (≥20%) reported with OPDIVO (n=206)
vs dacarbazine (n=205) were fatigue (49% vs 39%), musculoskeletal
pain (32% vs 25%), rash (28% vs 12%), and pruritus (23% vs 12%). In
Checkmate 067, the most common (≥20%) adverse reactions in the
OPDIVO plus YERVOY arm (n=313) were fatigue (62%), diarrhea (54%),
rash (53%), nausea (44%), pyrexia (40%), pruritus (39%),
musculoskeletal pain (32%), vomiting (31%), decreased appetite
(29%), cough (27%), headache (26%), dyspnea (24%), upper
respiratory tract infection (23%), arthralgia (21%), and increased
transaminases (25%). In Checkmate 067, the most common (≥20%)
adverse reactions in the OPDIVO arm (n=313) were fatigue (59%),
rash (40%), musculoskeletal pain (42%), diarrhea (36%), nausea
(30%), cough (28%), pruritus (27%), upper respiratory tract
infection (22%), decreased appetite (22%), headache (22%),
constipation (21%), arthralgia (21%), and vomiting (20%). In
Checkmate 238, the most common adverse reactions (≥20%) reported in
OPDIVO-treated patients (n=452) vs ipilimumab-treated patients
(n=453) were fatigue (57% vs 55%), diarrhea (37% vs 55%), rash (35%
vs 47%), musculoskeletal pain (32% vs 27%), pruritus (28% vs 37%),
headache (23% vs 31%), nausea (23% vs 28%), upper respiratory
infection (22% vs 15%), and abdominal pain (21% vs 23%). The most
common immune-mediated adverse reactions were rash (16%),
diarrhea/colitis (6%), and hepatitis (3%). In Checkmate 816, the
most common (>20%) adverse reactions in the OPDIVO plus
chemotherapy arm (n=176) were nausea (38%), constipation (34%),
fatigue (26%), decreased appetite (20%), and rash (20%). In
Checkmate 77T, the most common adverse reactions (reported in ≥20%)
in patients receiving OPDIVO in combination with chemotherapy (n=
228) were anemia (39.5%), constipation (32.0%), nausea (28.9%),
fatigue (28.1%), alopecia (25.9%), and cough (21.9%). In Checkmate
227, the most common (≥20%) adverse reactions were fatigue (44%),
rash (34%), decreased appetite (31%), musculoskeletal pain (27%),
diarrhea/colitis (26%), dyspnea (26%), cough (23%), hepatitis
(21%), nausea (21%), and pruritus (21%). In Checkmate 9LA, the most
common (>20%) adverse reactions were fatigue (49%),
musculoskeletal pain (39%), nausea (32%), diarrhea (31%), rash
(30%), decreased appetite (28%), constipation (21%), and pruritus
(21%). In Checkmate 017 and 057, the most common adverse reactions
(≥20%) in patients receiving OPDIVO (n=418) were fatigue,
musculoskeletal pain, cough, dyspnea, and decreased appetite. In
Checkmate 743, the most common adverse reactions (≥20%) in patients
receiving OPDIVO plus YERVOY were fatigue (43%), musculoskeletal
pain (38%), rash (34%), diarrhea (32%), dyspnea (27%), nausea
(24%), decreased appetite (24%), cough (23%), and pruritus (21%).
In Checkmate 214, the most common adverse reactions (≥20%) reported
in patients treated with OPDIVO plus YERVOY (n=547) were fatigue
(58%), rash (39%), diarrhea (38%), musculoskeletal pain (37%),
pruritus (33%), nausea (30%), cough (28%), pyrexia (25%),
arthralgia (23%), decreased appetite (21%), dyspnea (20%), and
vomiting (20%). In Checkmate 9ER, the most common adverse reactions
(≥20%) in patients receiving OPDIVO and cabozantinib (n=320) were
diarrhea (64%), fatigue (51%), hepatotoxicity (44%), palmar-plantar
erythrodysaesthesia syndrome (40%), stomatitis (37%), rash (36%),
hypertension (36%), hypothyroidism (34%), musculoskeletal pain
(33%), decreased appetite (28%), nausea (27%), dysgeusia (24%),
abdominal pain (22%), cough (20%) and upper respiratory tract
infection (20%). In Checkmate 025, the most common adverse
reactions (≥20%) reported in patients receiving OPDIVO (n=406) vs
everolimus (n=397) were fatigue (56% vs 57%), cough (34% vs 38%),
nausea (28% vs 29%), rash (28% vs 36%), dyspnea (27% vs 31%),
diarrhea (25% vs 32%), constipation (23% vs 18%), decreased
appetite (23% vs 30%), back pain (21% vs 16%), and arthralgia (20%
vs 14%). In Checkmate 141, the most common adverse reactions (≥10%)
in patients receiving OPDIVO (n=236) were cough (14%) and dyspnea
(14%) at a higher incidence than investigator’s choice. In
Checkmate 275, the most common adverse reactions (≥20%) reported in
patients receiving OPDIVO (n=270) were fatigue (46%),
musculoskeletal pain (30%), nausea (22%), and decreased appetite
(22%). In Checkmate 274, the most common adverse reactions (≥20%)
reported in patients receiving OPDIVO (n=351) were rash (36%),
fatigue (36%), diarrhea (30%), pruritus (30%), musculoskeletal pain
(28%), and urinary tract infection (22%).In Checkmate 901, the most
common adverse reactions (≥20%) were nausea, fatigue,
musculoskeletal pain, constipation, decreased appetite, rash,
vomiting, and peripheral neuropathy. In Attraction-3, the most
common adverse reactions (≥20%) in OPDIVO-treated patients (n=209)
were rash (22%) and decreased appetite (21%). In Checkmate 577, the
most common adverse reactions (≥20%) in patients receiving OPDIVO
(n=532) were fatigue (34%), diarrhea (29%), nausea (23%), rash
(21%), musculoskeletal pain (21%), and cough (20%). In Checkmate
648, the most common adverse reactions (≥20%) in patients treated
with OPDIVO in combination with chemotherapy (n=310) were nausea
(65%), decreased appetite (51%), fatigue (47%), constipation (44%),
stomatitis (44%), diarrhea (29%), and vomiting (23%). In Checkmate
648, the most common adverse reactions reported in ≥20% of patients
treated with OPDIVO in combination with YERVOY were rash (31%),
fatigue (28%), pyrexia (23%), nausea (22%), diarrhea (22%), and
constipation (20%). In Checkmate 649, the most common adverse
reactions (≥20%) in patients treated with OPDIVO in combination
with chemotherapy (n=782) were peripheral neuropathy (53%), nausea
(48%), fatigue (44%), diarrhea (39%), vomiting (31%), decreased
appetite (29%), abdominal pain (27%), constipation (25%), and
musculoskeletal pain (20%). In Checkmate 76K, the most common
adverse reactions (≥20%) reported with OPDIVO (n=524) were fatigue
(36%), musculoskeletal pain (30%), rash (28%), diarrhea (23%) and
pruritis (20%).
Surgery Related Adverse Reactions
In Checkmate 77T, 5.3% (n=12) of the OPDIVO-treated patients who
received neoadjuvant treatment, did not receive surgery due to
adverse reactions. The adverse reactions that led to cancellation
of surgery in OPDIVO- treated patients were cerebrovascular
accident, pneumonia, and colitis/diarrhea (2 patients each) and
acute coronary syndrome, myocarditis, hemoptysis, pneumonitis,
COVID-19, and myositis (1 patient each).
Please see U.S. Full Prescribing Information for OPDIVO and
YERVOY.
INDICATIONS
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the first-line treatment of adult patients with
intermediate or poor risk advanced renal cell carcinoma (RCC),
following treatment with intravenous nivolumab and ipilimumab
combination therapy.
Limitations of Use: OPDIVO QVANTIG is not indicated in
combination with ipilimumab for the treatment of renal cell
carcinoma.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), in combination
with cabozantinib, is indicated for the first- line treatment of
adult patients with advanced renal cell carcinoma (RCC).
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the treatment of adult patients with advanced
renal cell carcinoma (RCC) who have received prior anti-angiogenic
therapy.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the treatment of adult patients with unresectable
or metastatic melanoma.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the treatment of adult patients with unresectable
or metastatic melanoma following treatment with intravenous
nivolumab and ipilimumab combination therapy.
Limitations of Use: OPDIVO QVANTIG is not indicated in
combination with ipilimumab for treatment of unresectable or
metastatic melanoma.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the adjuvant treatment of adult patients with
completely resected Stage IIB, Stage IIC, Stage III, or Stage IV
melanoma.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), in combination
with platinum-doublet chemotherapy, is indicated as neoadjuvant
treatment of adult patients with resectable (tumors ≥4 cm or node
positive) non-small cell lung cancer (NSCLC).
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), in combination
with platinum-doublet chemotherapy, is indicated for the
neoadjuvant treatment of adult patients with resectable (tumors
>/=4 cm or node positive) non- small cell lung cancer (NSCLC)
and no known epidermal growth factor receptor (EGFR) mutations or
anaplastic lymphoma kinase (ALK) rearrangements, followed by
single-agent OPDIVO QVANTIG as monotherapy in the adjuvant setting
after surgical resection.
OPDIVO QVANTIG ™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the treatment of adult patients with metastatic
non-small cell lung cancer (NSCLC) with progression on or after
platinum-based chemotherapy. Patients with EGFR or ALK genomic
tumor aberrations should have disease progression on FDA-approved
therapy for these aberrations prior to receiving OPDIVO
QVANTIG.
Limitations of Use: OPDIVO QVANTIG is not indicated in
combination with ipilimumab for the treatment of metastatic
NSCLC.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the treatment of adult patients with recurrent or
metastatic squamous cell carcinoma of the head and neck (SCCHN)
with disease progression on or after platinum-based therapy.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the adjuvant treatment of adult patients with
urothelial carcinoma (UC) who are at high risk of recurrence after
undergoing radical resection of UC.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), in combination
with cisplatin and gemcitabine, is indicated for the first-line
treatment of adult patients with unresectable or metastatic
urothelial carcinoma (UC).
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the treatment of adult patients with locally
advanced or metastatic urothelial carcinoma (UC) who have disease
progression during or following platinum-containing chemotherapy or
have disease progression within 12 months of neoadjuvant or
adjuvant treatment with platinum-containing chemotherapy.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase), as monotherapy,
is indicated for the adjuvant treatment of completely resected
esophageal or gastroesophageal junction cancer with residual
pathologic disease in adult patients who have received neoadjuvant
chemoradiotherapy (CRT).
OPDIVO QVANTIG™ (nivolumab and hyaluronidase) in combination
with fluoropyrimidine- and platinum- containing chemotherapy, is
indicated for the first-line treatment of adult patients with
unresectable advanced or metastatic esophageal squamous cell
carcinoma (ESCC).
Limitations of Use: OPDIVO QVANTIG is not indicated in
combination with ipilimumab for the treatment of patients with
unresectable advanced or metastatic ESCC.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase) as monotherapy, is
indicated for the treatment of adult patients with unresectable
advanced, recurrent or metastatic esophageal squamous cell
carcinoma (ESCC) after prior fluoropyrimidine- and platinum-based
chemotherapy.
OPDIVO QVANTIG™ (nivolumab and hyaluronidase) in combination
with fluoropyrimidine- and platinum- containing chemotherapy, is
indicated for the treatment of adult patients with advanced or
metastatic gastric cancer, gastroesophageal junction cancer, and
esophageal adenocarcinoma.
IMPORTANT SAFETY INFORMATION
Severe and Fatal Immune-Mediated Adverse Reactions
Immune-mediated adverse reactions, which may be severe or fatal,
can occur in any organ system or tissue. While immune-mediated
adverse reactions usually manifest during treatment, they can also
occur after discontinuation of OPDIVO QVANTIG. Early identification
and management are essential to ensure safe use of OPDIVO QVANTIG.
Monitor for signs and symptoms that may be clinical manifestations
of underlying immune- mediated adverse reactions. Evaluate clinical
chemistries including liver enzymes, creatinine, and thyroid
function at baseline and periodically during treatment. In cases of
suspected immune-mediated adverse reactions, initiate appropriate
workup to exclude alternative etiologies, including infection.
Institute medical management promptly, including specialty
consultation as appropriate.
Withhold or permanently discontinue OPDIVO QVANTIG depending on
severity [please see Section 2 Dosage and Administration in the
accompanying Full Prescribing Information]. In general, if OPDIVO
QVANTIG interruption or discontinuation is required, administer
systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or
equivalent) until improvement to Grade 1 or less. Upon improvement
to Grade 1 or less, initiate corticosteroid taper and continue to
taper over for at least 1 month. Consider administration of other
systemic immunosuppressants in patients whose immune-mediated
adverse reactions are not controlled with corticosteroid
therapy.
Toxicity management guidelines for adverse reactions that do not
necessarily require systemic steroids (e.g., endocrinopathies and
dermatologic reactions) are discussed below.
Immune-Mediated Pneumonitis
OPDIVO QVANTIG can cause immune-mediated pneumonitis. The
incidence of pneumonitis is higher in patients who have received
prior thoracic radiation.
Immune-mediated pneumonitis occurred in 2.8% (7/247) of patients
receiving OPDIVO QVANTIG, including Grade 3 (0.8%) and Grade 2
(2.0%) adverse reactions.
Immune-Mediated Colitis
OPDIVO QVANTIG can cause immune-mediated colitis. A common
symptom included in the definition of colitis was diarrhea.
Cytomegalovirus (CMV) infection/reactivation has been reported in
patients with corticosteroid- refractory immune-mediated colitis.
In cases of corticosteroid-refractory colitis, consider repeating
infectious workup to exclude alternative etiologies.
Immune-mediated colitis occurred in 2.8% (7/247) of patients
receiving OPDIVO QVANTIG, including Grade 3 (0.4%) and Grade 2
(2.4%) adverse reactions.
Immune-Mediated Hepatitis and Hepatotoxicity
OPDIVO QVANTIG can cause immune-mediated hepatitis.
Immune-mediated hepatitis occurred in 2.4% (6/247) of patients
receiving OPDIVO QVANTIG, including Grade 3 (1.6%), and Grade 2
(0.8%) adverse reactions. Intravenous nivolumab in combination with
cabozantinib can cause hepatic toxicity with higher frequencies of
Grade 3 and 4 ALT and AST elevations compared to intravenous
nivolumab alone. Consider more frequent monitoring of liver enzymes
as compared to when the drugs are administered as single agents.
With the combination of intravenous nivolumab and cabozantinib,
Grades 3 and 4 increased ALT or AST were seen in 11% (35/320) of
patients.
Immune-Mediated Endocrinopathies
OPDIVO QVANTIG can cause primary or secondary adrenal
insufficiency, immune-mediated hypophysitis, immune-mediated
thyroid disorders, and Type 1 diabetes mellitus, which can present
with diabetic ketoacidosis. Withhold OPDIVO QVANTIG depending on
severity [please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information]. For Grade 2 or higher
adrenal insufficiency, initiate symptomatic treatment, including
hormone replacement as clinically indicated. Hypophysitis can
present with acute symptoms associated with mass effect such as
headache, photophobia, or visual field defects. Hypophysitis can
cause hypopituitarism; initiate hormone replacement as clinically
indicated. Thyroiditis can present with or without endocrinopathy.
Hypothyroidism can follow hyperthyroidism; initiate hormone
replacement or medical management as clinically indicated. Monitor
patients for hyperglycemia or other signs and symptoms of diabetes;
initiate treatment with insulin as clinically indicated.
Adrenal insufficiency occurred in 2% (5/247) of patients
receiving OPDIVO QVANTIG, including Grade 3 (0.8%) and Grade 2
(1.2%) adverse reactions. Adrenal insufficiency occurred in 4.7%
(15/320) of patients with RCC who received intravenous nivolumab
with cabozantinib, including Grade 3 (2.2%) and Grade 2 (1.9%)
adverse reactions. Hypophysitis occurred in 0.6% (12/1994) of
patients treated with single agent intravenous nivolumab, including
Grade 3 (0.2%) and Grade 2 (0.3%). Thyroiditis occurred in 0.4%
(1/247) of patients receiving OPDIVO QVANTIG, including a Grade 1
(0.4%) adverse reaction.
Hyperthyroidism occurred in 0.8% (2/247) of patients receiving
OPDIVO QVANTIG, including Grade 2 (0.4%) adverse reactions.
Hypothyroidism occurred in 9% (23/247) of patients receiving OPDIVO
QVANTIG, including Grade 2 (5.7%) adverse reactions.
Grade 3 diabetes occurred in 0.4% (1/247) of patients receiving
OPDIVO QVANTIG.
Immune-Mediated Nephritis with Renal Dysfunction
OPDIVO QVANTIG can cause immune-mediated nephritis.
Grade 2 immune-mediated nephritis and renal dysfunction occurred
in 1.2% (3/247) of patients receiving OPDIVO QVANTIG.
Immune-Mediated Dermatologic Adverse Reactions
OPDIVO QVANTIG can cause immune-mediated rash or dermatitis.
Exfoliative dermatitis, including Stevens- Johnson Syndrome, toxic
epidermal necrolysis (TEN), and DRESS (drug rash with eosinophilia
and systemic symptoms), has occurred with PD-1/PD-L1 blocking
antibodies. Topical emollients and/or topical corticosteroids may
be adequate to treat mild to moderate non-exfoliative rashes.
Withhold or permanently discontinue OPDIVO QVANTIG depending on
severity (please see section 2 Dosage and Administration in the
accompanying Full Prescribing Information).
Immune-mediated rash occurred in 7% (17/247) of patients,
including Grade 3 (0.8%) and Grade 2 (2.8%) adverse reactions.
Other Immune-Mediated Adverse Reactions
The following clinically significant immune-mediated adverse
reactions occurred at an incidence of <1% (unless otherwise
noted) in patients who received OPDIVO QVANTIG or intravenous
nivolumab as single agent or in combination with chemotherapy or
immunotherapy, or were reported with the use of other PD-1/PD-L1
blocking antibodies. Severe or fatal cases have been reported for
some of these adverse reactions: cardiac/vascular : myocarditis,
pericarditis, vasculitis; nervous system : meningitis,
encephalitis, myelitis and demyelination, myasthenic
syndrome/myasthenia gravis (including exacerbation), Guillain-Barré
syndrome, nerve paresis, autoimmune neuropathy; ocular : uveitis,
iritis, and other ocular inflammatory toxicities can occur;
gastrointestinal : pancreatitis to include increases in serum
amylase and lipase levels, gastritis, duodenitis; musculoskeletal
and connective tissue : myositis/polymyositis, rhabdomyolysis, and
associated sequelae including renal failure, arthritis, polymyalgia
rheumatica; endocrine : hypoparathyroidism; other
(hematologic/immune) : hemolytic anemia, aplastic anemia,
hemophagocytic lymphohistiocytosis (HLH), systemic inflammatory
response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi
lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, solid
organ transplant rejection, other transplant (including corneal
graft) rejection.
Some ocular IMAR cases can be associated with retinal
detachment. Various grades of visual impairment, including
blindness, can occur. If uveitis occurs in combination with other
immune-mediated adverse reactions, consider a
Vogt-Koyanagi-Harada–like syndrome, as this may require treatment
with systemic corticosteroids to reduce the risk of permanent
vision loss.
Complications of Allogeneic Hematopoietic Stem Cell
Transplantation
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with OPDIVO QVANTIG.
Transplant-related complications include hyperacute
graft-versus-host-disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease (VOD) after reduced intensity conditioning,
and steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between OPDIVO QVANTIG and allogeneic HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with OPDIVO QVANTIG prior to or after an
allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal studies,
OPDIVO QVANTIG can cause fetal harm when administered to a pregnant
woman. In animal reproduction studies, administration of nivolumab
to cynomolgus monkeys from the onset of organogenesis through
delivery resulted in increased abortion and premature infant death.
Advise pregnant women of the potential risk to a fetus. Advise
females of reproductive potential to use effective contraception
during treatment with OPDIVO QVANTIG and for 5 months after the
last dose.
Increased Mortality in Patients with Multiple Myeloma when
Nivolumab Is Added to a Thalidomide Analogue and
Dexamethasone
In randomized clinical trials in patients with multiple myeloma,
the addition of a PD-1 blocking antibody, including intravenous
nivolumab, to a thalidomide analogue plus dexamethasone, a use for
which no PD-1 or PD-L1 blocking antibody is indicated, resulted in
increased mortality. Treatment of patients with multiple myeloma
with a PD-1 or PD-L1 blocking antibody in combination with a
thalidomide analogue plus dexamethasone is not recommended outside
of controlled clinical trials.
Lactation
There are no data on the presence of nivolumab or hyaluronidase
in human milk, the effects on the breastfed child, or the effects
on milk production. Because of the potential for serious adverse
reactions in the breastfed child, advise women not to breastfeed
during treatment and for 5 months after the last dose of OPDIVO
QVANTIG.
Serious Adverse Reactions
In Checkmate 67T, serious adverse reactions occurred in 28% of
patients who received OPDIVO QVANTIG (n=247). Serious adverse
reactions in >1% of patients included pleural effusion (1.6%),
pneumonitis (1.6%), hyperglycemia (1.2%), hyperkalemia (1.2%),
hemorrhage (1.2%) and diarrhea (1.2%). Fatal adverse reactions
occurred in 3 patients (1.2%) who received OPDIVO QVANTIG and
included myocarditis, myositis, and colitis complications. In
Checkmate 037, serious adverse reactions occurred in 41% of
patients receiving intravenous nivolumab (n=268). Grade 3 and 4
adverse reactions occurred in 42% of patients receiving intravenous
nivolumab. The most frequent Grade 3 and 4 adverse drug reactions
reported in 2% to <5% of patients receiving intravenous
nivolumab were abdominal pain, hyponatremia, increased aspartate
aminotransferase, and increased lipase. In Checkmate 066, serious
adverse reactions occurred in 36% of patients receiving intravenous
nivolumab (n=206). Grade 3 and 4 adverse reactions occurred in 41%
of patients receiving intravenous nivolumab. The most frequent
Grade 3 and 4 adverse reactions reported in ≥2% of patients
receiving intravenous nivolumab were gamma-glutamyltransferase
increase (3.9%) and diarrhea (3.4%). In Checkmate 067, the most
frequent (≥10%) serious adverse reactions in the intravenous
nivolumab arm (n=313) were diarrhea (2.2%), colitis (1.9%), and
pyrexia (1.0%). In Checkmate 067, serious adverse reactions (74%
and 44%), adverse reactions leading to permanent discontinuation
(47% and 18%) or to dosing delays (58% and 36%), and Grade 3 or 4
adverse reactions (72% and 51%) all occurred more frequently in the
intravenous nivolumab plus intravenous ipilimumab arm (n=313)
relative to the intravenous nivolumab arm (n=313). The most
frequent (≥10%) serious adverse reactions in the intravenous
nivolumab plus intravenous ipilimumab arm and the intravenous
nivolumab arm, respectively, were diarrhea (13% and 2.2%), colitis
(10% and 1.9%), and pyrexia (10% and 1.0%).
In Checkmate 816, serious adverse reactions occurred in 30% of
patients (n=176) who were treated with intravenous nivolumab in
combination with platinum-doublet chemotherapy. Serious adverse
reactions in >2% included pneumonia and vomiting. No fatal
adverse reactions occurred in patients who received intravenous
nivolumab in combination with platinum-doublet chemotherapy. In
Checkmate 77T, serious adverse reactions occurred in 21% of
patients who received intravenous nivolumab in combination with
platinum-doublet chemotherapy as neoadjuvant treatment (n=228). The
most frequent (≥2%) serious adverse reactions was pneumonia. Fatal
adverse reactions occurred in 2.2% of patients, due to
cerebrovascular accident, COVID-19 infection, hemoptysis,
pneumonia, and pneumonitis (0.4% each). In the adjuvant phase of
Checkmate 77T, 22% of patients experienced serious adverse
reactions (n=142). The most frequent serious adverse reaction was
pneumonitis/ILD (2.8%). One fatal adverse reaction due to COVID-19
occurred. In Checkmate 017 and 057, serious adverse reactions
occurred in 46% of patients receiving intravenous nivolumab
(n=418). The most frequent serious adverse reactions reported in
≥2% of patients receiving intravenous nivolumab were pneumonia,
pulmonary embolism, dyspnea, pyrexia, pleural effusion,
pneumonitis, and respiratory failure. In Checkmate 057, fatal
adverse reactions occurred; these included events of infection (7
patients, including one case of Pneumocystis jirovecii pneumonia),
pulmonary embolism (4 patients), and limbic encephalitis (1
patient). In Checkmate 214, serious adverse reactions occurred in
59% of patients receiving intravenous nivolumab plus intravenous
ipilimumab (n=547). The most frequent serious adverse reactions
reported in ≥2% of patients were diarrhea, pyrexia, pneumonia,
pneumonitis, hypophysitis, acute kidney injury, dyspnea, adrenal
insufficiency, and colitis. In Checkmate 9ER, serious adverse
reactions occurred in 48% of patients receiving intravenous
nivolumab and cabozantinib (n=320). The most frequent serious
adverse reactions reported in ≥2% of patients were diarrhea,
pneumonia, pneumonitis, pulmonary embolism, urinary tract
infection, and hyponatremia. Fatal intestinal perforations occurred
in 3 (0.9%) patients. In Checkmate 025, serious adverse reactions
occurred in 47% of patients receiving intravenous nivolumab
(n=406). The most frequent serious adverse reactions reported in
≥2% of patients were acute kidney injury, pleural effusion,
pneumonia, diarrhea, and hypercalcemia. In Checkmate 141, serious
adverse reactions occurred in 49% of patients receiving intravenous
nivolumab (n=236). The most frequent serious adverse reactions
reported in ≥2% of patients receiving intravenous nivolumab were
pneumonia, dyspnea, respiratory failure, respiratory tract
infection, and sepsis. In Checkmate 275, serious adverse reactions
occurred in 54% of patients receiving intravenous nivolumab
(n=270). The most frequent serious adverse reactions reported in ≥
2% of patients receiving intravenous nivolumab were urinary tract
infection, sepsis, diarrhea, small intestine obstruction, and
general physical health deterioration. In Checkmate 274, serious
adverse reactions occurred in 30% of patients receiving intravenous
nivolumab (n=351). The most frequent serious adverse reaction
reported in ≥ 2% of patients receiving intravenous nivolumab was
urinary tract infection. Fatal adverse reactions occurred in 1% of
patients; these included events of pneumonitis (0.6%). In Checkmate
901, serious adverse reactions occurred in 48% of patients
receiving intravenous nivolumab in combination with chemotherapy.
The most frequent serious adverse reactions reported in ≥2% of
patients who received intravenous nivolumab with chemotherapy were
urinary tract infection (4.9%), acute kidney injury (4.3%), anemia
(3%), pulmonary embolism (2.6%), sepsis (2.3%), and platelet count
decreased (2.3%). Fatal adverse reactions occured in 3.6% of
patients who received intravenous nivolumab in combination with
chemotherapy; these included sepsis (1%). In Checkmate 238, serious
adverse reactions occurred in 18% of patients receiving intravenous
nivolumab (n=452). Grade 3 or 4 adverse reactions occurred in 25%
of intravenous nivolumab-treated patients (n=452). The most
frequent Grade 3 and 4 adverse reactions reported in ≥2% of
intravenous nivolumab-treated patients were diarrhea and increased
lipase and amylase. In Attraction-3, serious adverse reactions
occurred in 38% of patients receiving intravenous nivolumab
(n=209). Serious adverse reactions reported in ≥2% of patients who
received intravenous nivolumab were pneumonia, esophageal fistula,
interstitial lung disease, and pyrexia. The following fatal adverse
reactions occurred in patients who received intravenous nivolumab:
interstitial lung disease or pneumonitis (1.4%), pneumonia (1.0%),
septic shock (0.5%), esophageal fistula (0.5%), gastrointestinal
hemorrhage (0.5%), pulmonary embolism (0.5%), and sudden death
(0.5%). In Checkmate 577, serious adverse reactions occurred in 33%
of patients receiving intravenous nivolumab (n=532). A serious
adverse reaction reported in ≥2% of patients who received
intravenous nivolumab was pneumonitis. A fatal reaction of
myocardial infarction occurred in one patient who received
intravenous nivolumab. In Checkmate 648, serious adverse reactions
occurred in 62% of patients receiving intravenous nivolumab in
combination with chemotherapy (n=310). The most frequent serious
adverse reactions reported in ≥2% of patients who received
intravenous nivolumab with chemotherapy were pneumonia (11%),
dysphagia (7%), esophageal stenosis (2.9%), acute kidney injury
(2.9%), and pyrexia (2.3%). Fatal pneumonitis, pneumatosis
intestinalis, pneumonia, and acute kidney injury. In Checkmate 648,
serious adverse reactions occurred in 69% of patients receiving
intravenous nivolumab in combination with intravenous ipilimumab
(n=322). The most frequent serious adverse reactions reported in
≥2% who received intravenous nivolumab in combination with
intravenous ipilimumab were pneumonia (10 %), pyrexia (4.3%),
pneumonitis (4.0%), aspiration pneumonia (3.7%), dysphagia (3.7%),
hepatic function abnormal (2.8%), decreased appetite (2.8%),
adrenal insufficiency (2.5%), and dehydration (2.5%). Fatal adverse
reactions occurred in 5 (1.6%) patients who received intravenous
nivolumab in combination with intravenous ipilimumab; these
included pneumonitis, interstitial lung disease, pulmonary
embolism, and acute respiratory distress syndrome. In Checkmate
649, serious adverse reactions occurred in 52% of patients treated
with intravenous nivolumab in combination with chemotherapy
(n=782). The most frequent serious adverse reactions reported in ≥
2% of patients treated with intravenous nivolumab in combination
with chemotherapy were vomiting (3.7%), pneumonia (3.6%), anemia,
(3.6%), pyrexia (2.8%), diarrhea (2.7%), febrile neutropenia
(2.6%), and pneumonitis (2.4%). Fatal adverse reactions occurred in
16 (2.0%) patients who were treated with intravenous nivolumab in
combination with chemotherapy; these included pneumonitis (4
patients), febrile neutropenia (2 patients), stroke (2 patients),
gastrointestinal toxicity, intestinal mucositis, septic shock,
pneumonia, infection, gastrointestinal bleeding, mesenteric vessel
thrombosis, and disseminated intravascular coagulation. In
Checkmate 76K, serious adverse reactions occurred in 18% of
patients receiving intravenous nivolumab (n=524). Adverse reactions
which resulted in permanent discontinuation of intravenous
nivolumab in >1% of patients included arthralgia (1.7%), rash
(1.7%), and diarrhea (1.1%). A fatal adverse reaction occurred in 1
(0.2%) patient (heart failure and acute kidney injury). The most
frequent Grade 3-4 lab abnormalities reported in ≥1% of intravenous
nivolumab-treated patients were increased lipase (2.9%), increased
AST (2.2%), increased ALT (2.1%), lymphopenia (1.1%), and decreased
potassium (1.0%).
Common Adverse Reactions
In Checkmate 67T, the most common adverse reactions (≥10%) in
patients treated with OPDIVO QVANTIG (n=247) were musculoskeletal
pain (31%), fatigue (20%), pruritus (16%), rash (15%),
hypothyroidism (12%), diarrhea (11%), cough (11%), and abdominal
pain (10%). In Checkmate 037, the most common adverse reaction
(≥20%) reported with intravenous nivolumab (n=268) was rash (21%).
In Checkmate 066, the most common adverse reactions (≥20%) reported
with intravenous nivolumab (n=206) vs dacarbazine (n=205) were
fatigue (49% vs 39%), musculoskeletal pain (32% vs 25%), rash (28%
vs 12%), and pruritus (23% vs 12%). In Checkmate 067, the most
common (≥20%) adverse reactions in the intravenous nivolumab arm
(n=313) were fatigue (59%), rash (40%), musculoskeletal pain (42%),
diarrhea (36%), nausea (30%), cough (28%), pruritus (27%), upper
respiratory tract infection (22%), decreased appetite (22%),
headache (22%), constipation (21%), arthralgia (21%), and vomiting
(20%). In Checkmate 067, the most common (≥20%) adverse reactions
in the intravenous nivolumab plus intravenous ipilimumab arm
(n=313) were fatigue (62%), diarrhea (54%), rash (53%), nausea
(44%), pyrexia (40%), pruritus (39%), musculoskeletal pain (32%),
vomiting (31%), decreased appetite (29%), cough (27%), headache
(26%), dyspnea (24%), upper respiratory tract infection (23%),
arthralgia (21%), and increased transaminases (25%).
In Checkmate 816, the most common (>20%) adverse reactions in
the intravenous nivolumab plus chemotherapy arm (n=176) were nausea
(38%), constipation (34%), fatigue (26%), decreased appetite (20%),
and rash (20%).In Checkmate 77T, the most common adverse reactions
(reported in ≥20%) in patients receiving intravenous nivolumab in
combination with chemotherapy (n= 228) were anemia (39.5%),
constipation (32.0%), nausea (28.9%), fatigue (28.1%), alopecia
(25.9%), and cough (21.9%).In Checkmate 017 and 057, the most
common adverse reactions (≥20%) in patients receiving intravenous
nivolumab (n=418) were fatigue, musculoskeletal pain, cough,
dyspnea, and decreased appetite. In Checkmate 214, the most common
adverse reactions (≥20%) reported in patients treated with
intravenous nivolumab plus intravenous ipilimumab (n=547) were
fatigue (58%), rash (39%), diarrhea (38%), musculoskeletal pain
(37%), pruritus (33%), nausea (30%), cough (28%), pyrexia (25%),
arthralgia (23%), decreased appetite (21%), dyspnea (20%), and
vomiting (20%). In Checkmate 9ER, the most common adverse reactions
(≥20%) in patients receiving intravenous nivolumab and cabozantinib
(n=320) were diarrhea (64%), fatigue (51%), hepatotoxicity (44%),
palmar-plantar erythrodysaesthesia syndrome (40%), stomatitis
(37%), rash (36%), hypertension (36%), hypothyroidism (34%),
musculoskeletal pain (33%), decreased appetite (28%), nausea (27%),
dysgeusia (24%), abdominal pain (22%), cough (20%) and upper
respiratory tract infection (20%). In Checkmate 025, the most
common adverse reactions (≥20%) reported in patients receiving
intravenous nivolumab (n=406) vs everolimus (n=397) were fatigue
(56% vs 57%), cough (34% vs 38%), nausea (28% vs 29%), rash (28% vs
36%), dyspnea (27% vs 31%), diarrhea (25% vs 32%), constipation
(23% vs 18%), decreased appetite (23% vs 30%), back pain (21% vs
16%), and arthralgia (20% vs 14%).In Checkmate 141, the most common
adverse reactions (≥10%) in patients receiving intravenous
nivolumab (n=236) were cough (14%) and dyspnea (14%) at a higher
incidence than investigator’s choice. In Checkmate 275, the most
common adverse reactions (≥ 20%) reported in patients receiving
intravenous nivolumab (n=270) were fatigue (46%), musculoskeletal
pain (30%), nausea (22%), and decreased appetite (22%).In Checkmate
274, the most common adverse reactions (20%) reported in patients
receiving intravenous nivolumab (n=351) were rash (36%), fatigue
(36%), diarrhea (30%), pruritus (30%), musculoskeletal pain (28%),
and urinary tract infection (22%). In Checkmate 901, The most
common adverse reactions (reported in ≥20% of patients) were nausea
(52%), fatigue (48%), musculoskeletal pain (33%), constipation
(30%), decreased appetite (30%), rash (25%), vomiting (23%), and
peripheral neuropathy (20%). In Checkmate 238, the most common
adverse reactions (≥20%) reported in intravenous nivolumab-treated
patients (n=452) vs ipilimumab-treated patients (n=453) were
fatigue (57% vs 55%), diarrhea (37% vs 55%), rash (35% vs 47%),
musculoskeletal pain (32% vs 27%), pruritus (28% vs 37%), headache
(23% vs 31%), nausea (23% vs 28%), upper respiratory infection (22%
vs 15%), and abdominal pain (21% vs 23%). The most common
immune-mediated adverse reactions were rash (16%), diarrhea/colitis
(6%), and hepatitis (3%).In Attraction-3, the most common adverse
reactions (≥20%) in intravenous nivolumab-treated patients (n=209)
were rash (22%) and decreased appetite (21%).In Checkmate 577, the
most common adverse reactions (≥20%) in patients receiving
intravenous nivolumab (n=532) were fatigue (34%), diarrhea (29%),
nausea (23%), rash (21%), musculoskeletal pain (21%), and cough
(20%).In Checkmate 648, the most common adverse reactions (≥20%) in
patients treated with intravenous nivolumab in combination with
chemotherapy (n=310) were nausea (65%), decreased appetite (51%),
fatigue (47%), constipation (44%), stomatitis (44%), fatigue (32%),
diarrhea (29%), and vomiting (23%). In Checkmate 648, the most
common adverse reactions reported in ≥20% of patients treated with
intravenous nivolumab in combination with intravenous ipilimumab
were rash (31%), fatigue (28 %), pyrexia (23%), nausea (22%),
diarrhea (22%), fatigue (21%), and constipation (20%). In Checkmate
649, the most common adverse reactions (≥ 20%) in patients treated
with intravenous nivolumab in combination with chemotherapy (n=782)
were peripheral neuropathy (53%), nausea (48%), fatigue (44%),
diarrhea (39%), vomiting (31%), decreased appetite (29%), abdominal
pain (27%), constipation (25%), and musculoskeletal pain (20%).In
Checkmate 76K, the most common adverse reactions (≥20%) reported
with intravenous nivolumab (n=524) were fatigue (36%),
musculoskeletal pain (30%), rash (28%), diarrhea (23%) and pruritis
(20%).
Surgery Related Adverse Reactions
In Checkmate 77T, 5.3% (n=12) of the intravenous
nivolumab-treated patients who received neoadjuvant treatment, did
not receive surgery due to adverse reactions. The adverse reactions
that led to cancellation of surgery in intravenous
nivolumab-treated patients were cerebrovascular accident,
pneumonia, and colitis/diarrhea (2 patients each) and acute
coronary syndrome, myocarditis, hemoptysis, pneumonitis, COVID-19,
and myositis (1 patient each).
Please see U.S. Full Prescribing Information for OPDIVO
QVANTIG.
Bristol Myers Squibb: Creating a Better
Future for People with Cancer Bristol Myers Squibb is
inspired by a single vision — transforming patients’ lives through
science. The goal of the company’s cancer research is to deliver
medicines that offer each patient a better, healthier life and to
make cure a possibility. Building on a legacy across a broad range
of cancers that have changed survival expectations for many,
Bristol Myers Squibb researchers are exploring new frontiers in
personalized medicine and, through innovative digital platforms,
are turning data into insights that sharpen their focus. Deep
understanding of causal human biology, cutting-edge capabilities
and differentiated research programs uniquely position the company
to approach cancer from every angle.
Cancer can have a relentless grasp on many parts of a patient’s
life, and Bristol Myers Squibb is committed to taking actions to
address all aspects of care, from diagnosis to survivorship. As a
leader in cancer care, Bristol Myers Squibb is working to empower
all people with cancer to have a better future.
About the Bristol Myers Squibb and Ono
Pharmaceutical Collaboration
In 2011, through a collaboration agreement with Ono
Pharmaceutical Co., Bristol Myers Squibb expanded its territorial
rights to develop and commercialize Opdivo globally, except in
Japan, South Korea and Taiwan, where Ono had retained all rights to
the compound at the time. On July 23, 2014, Ono and Bristol Myers
Squibb further expanded the companies’ strategic collaboration
agreement to jointly develop and commercialize multiple
immunotherapies – as single agents and combination regimens – for
patients with cancer in Japan, South Korea and Taiwan.
About Bristol Myers
Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, X, YouTube, Facebook and Instagram.
Cautionary Statement Regarding
Forward-Looking Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on current expectations and projections about our future
financial results, goals, plans and objectives and involve inherent
risks, assumptions and uncertainties, including internal or
external factors that could delay, divert or change any of them in
the next several years, that are difficult to predict, may be
beyond our control and could cause our future financial results,
goals, plans and objectives to differ materially from those
expressed in, or implied by, the statements. These risks,
assumptions, uncertainties and other factors include, among others,
the possibility of unfavorable results from further clinical trials
involving Opdualag (nivolumab and relatlimab-rmbw) and whether
Opdualag for the additional indication described in this release
will be successfully developed and commercialized. No
forward-looking statement can be guaranteed. Forward-looking
statements in this press release should be evaluated together with
the many risks and uncertainties that affect Bristol Myers Squibb’s
business and market, particularly those identified in the
cautionary statement and risk factors discussion in Bristol Myers
Squibb’s Annual Report on Form 10-K for the year ended December 31,
2024, as updated by our subsequent Quarterly Reports on Form 10-Q,
Current Reports on Form 8-K and other filings with the Securities
and Exchange Commission. The forward-looking statements included in
this document are made only as of the date of this document and
except as otherwise required by applicable law, Bristol Myers
Squibb undertakes no obligation to publicly update or revise any
forward-looking statement, whether as a result of new information,
future events, changed circumstances or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20250213295909/en/
Bristol Myers Squibb
Media Inquiries: Media@BMS.com
Investors: Investor.relations@bms.com
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
From Jan 2025 to Feb 2025
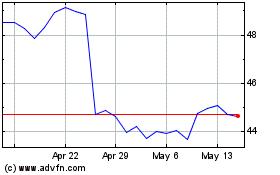
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
From Feb 2024 to Feb 2025