- New launches reinforce Baxter’s leadership in bringing
high-value, specialty injectable products to market to help address
critical patient needs
- Products help support patient safety, simplify medication
preparation and increase efficiencies for healthcare
professionals
- Marks total of 10 launches1 for Baxter’s U.S. Pharmaceuticals
portfolio in 2024
Baxter International Inc. (NYSE:BAX), a global leader in
injectables, anesthesia and drug compounding, today announced five
new injectable pharmaceutical product launches in the U.S., joining
the previous five launches announced in April of this year and
marking a total of 10 U.S. injectable product launches in 2024.
“Our Pharmaceuticals teams are relentlessly focused on bringing
differentiated products to market that support our customers in
helping to address vital patient needs,” said Alok Sonig, executive
vice president and group president, Pharmaceuticals, at Baxter. “We
look forward to further accelerating our impact with a robust
innovation pipeline across our key therapeutic areas, including
critical care, anti-infectives, pain and oncology.”
The five recent product launches within Baxter’s Pharmaceuticals
portfolio in the U.S. include the following. For all products,
please see full Indications, including Limitations of Use,
Important Risk Information and links to full Prescribing
Information below.
- Micafungin in 0.9% Sodium Chloride Injection single-dose
container is indicated for use in adult and pediatric patients to
treat Candida infections and for prophylaxis of Candida infections
in patients undergoing hematopoietic stem cell transplantation for
whom appropriate dosing with this formulation can be achieved.
Micafungin uses Baxter’s proprietary container technology. Baxter
offers Micafungin in 50 mg/50 mL, 100 mg/100 mL and 150 mg/150 mL
strengths.
- Cyclophosphamide Injection is an alkylating drug indicated for
treatment of adults and pediatric patients with various malignant
diseases and is frequently used in combination with other oncology
medications. This liquid cyclophosphamide product requires further
dilution before use. Baxter offers Cyclophosphamide Injection in
500 mg/2.5 mL and 1000 mg/5 mL strengths in Multiple-Dose
Vials.
- Pantoprazole Sodium in 0.9% Sodium Chloride Injection is a
proton pump inhibitor indicated in adults for the short-term
treatment (seven to 10 days) of gastroesophageal reflux disease
(GERD) associated with a history of erosive esophagitis (EE) and
pathological hypersecretion conditions including Zollinger-Ellison
(ZE) Syndrome. Pantoprazole uses Baxter’s proprietary container
technology. Baxter offers Pantoprazole in 40 mg/50 mL, 40 mg/100 mL
and 80 mg/100 mL strengths.
- Cefazolin in Dextrose Injection, USP now available in a new 3
g/150 mL strength, is a single-dose, first generation cephalosporin
antibacterial indicated for adults and pediatric patients to treat
various infections caused by susceptible organisms and for
perioperative prophylaxis. Cefazolin uses Baxter’s proprietary
container technology. Baxter offers Cefazolin in 1 g/50 mL, 2 g/100
mL and 3 g/150 mL strengths.
- Levetiracetam in Sodium Chloride Injection is an anti-epileptic
drug indicated for adjunct therapy in adult patients for partial
onset seizures, myoclonic seizures, and tonic-clonic seizures.
Levetiracetam uses Baxter’s proprietary container technology and is
now offered in 500 mg/100 mL, 1000 mg/100 mL and 1500 mg/100 mL
strengths.
Ready-to-use formats of standard concentrations of commonly
prescribed drugs may offer operational efficiencies for healthcare
providers. Compounding a drug for patient use is a multi-step,
manual process that requires oversight by pharmacy staff. A
ready-to-use product can simplify the preparation process and
support patient safety by reducing the chance of contamination2 and
avoiding potential errors that may occur when medications are
compounded.3
These five newly launched products are now available for use in
the U.S.
About Baxter Pharmaceuticals
Baxter is a global leader in specialty injectables, drug
compounding and anesthesia that addresses unmet patient needs in
the therapeutic areas of pain, critical care, anti-infectives and
oncology. Baxter’s comprehensive pharmaceuticals portfolio contains
injectables (including ready-to-use products), inhaled gases and
compounded medications, and is designed to expand access to
products that simplify medication preparation and support patient
safety. Pharmaceuticals employees across the globe are focused on
driving customer-centered innovation, bringing new and
differentiated products and delivery platforms to market, and
helping patients receive the medications they need.
About Baxter
Every day, millions of patients, caregivers and healthcare
providers rely on Baxter’s leading portfolio of diagnostic,
critical care, kidney care, nutrition, hospital and surgical
products used across patient homes, hospitals, physician offices
and other sites of care. For more than 90 years, we’ve been
operating at the critical intersection where innovations that save
and sustain lives meet the healthcare providers who make it happen.
With products, digital health solutions and therapies available in
more than 100 countries, Baxter’s employees worldwide are now
building upon the company’s rich heritage of medical breakthroughs
to advance the next generation of transformative healthcare
innovations. To learn more, visit www.baxter.com and follow us on
X, LinkedIn and Facebook.
Micafungin in 0.9% Sodium Chloride Injection
Indications
- Micafungin in Sodium Chloride Injection is an echinocandin
indicated in adult and pediatric patients for:
- Treatment of Candidemia, Acute Disseminated Candidiasis,
Candida Peritonitis and Abscesses in adult and pediatric patients 4
months of age and older for whom appropriate dosing with this
formulation can be achieved.
- Treatment of Candidemia, Acute Disseminated Candidiasis,
Candida Peritonitis and Abscesses without meningoencephalitis
and/or ocular dissemination in pediatric patients younger than 4
months of age for whom appropriate dosing with this formulation can
be achieved.
- Treatment of Esophageal Candidiasis in adult and pediatric
patients 4 months of age and older for whom appropriate dosing with
this formulation can be achieved.
- Prophylaxis of Candida Infections in adult and pediatric
patients 4 months of age and older undergoing Hematopoietic Stem
Cell Transplantation (HSCT) for whom appropriate dosing with this
formulation can be achieved.
- Limitations of Use:
- The safety and effectiveness of Micafungin in Sodium Chloride
Injection have not been established
for the treatment of candidemia with
meningoencephalitis and/or ocular dissemination in pediatric
patients younger than 4 months of age as a higher dose may be
needed.
- Micafungin in Sodium Chloride Injection has not been adequately
studied in patients with endocarditis, osteomyelitis or
meningoencephalitis due to Candida.
- The efficacy of Micafungin in Sodium Chloride Injection against
infections caused by fungi other than Candida has not been
established.
Important Risk Information
- Contraindications: Micafungin in Sodium Chloride Injection is
contraindicated in persons with known hypersensitivity to
micafungin sodium, any component of Micafungin in Sodium Chloride
Injection, or other echinocandins.
- Hypersensitivity Reactions: Anaphylaxis and anaphylactoid
reactions (including shock) have been observed. Discontinue
Micafungin in Sodium Chloride Injection and administer appropriate
treatment.
- Hematological Effects: Acute intravascular hemolysis and
hemoglobinuria was seen in a healthy volunteer during infusion of
Micafungin for Injection (200 mg) and oral prednisolone (20 mg).
Cases of significant hemolysis and hemolytic anemia have also been
reported in patients treated with Micafungin for Injection.
Patients who develop clinical or laboratory evidence of hemolysis
or hemolytic anemia during therapy should be monitored closely for
evidence of worsening of these conditions and evaluated for the
risk/benefit of continuing therapy.
- Hepatic Effects: Laboratory abnormalities in liver function
tests have been seen in healthy volunteers and patients treated
with Micafungin. In some patients with serious underlying
conditions who were receiving Micafungin along with multiple
concomitant medications, clinical hepatic abnormalities have
occurred, and isolated cases of significant hepatic impairment,
hepatitis, and hepatic failure have been reported. Monitor hepatic
function. Discontinue if severe dysfunction occurs.
- Renal Effects: Elevations in BUN and creatinine; isolated cases
of renal impairment or acute renal failure have been reported.
Monitor renal function.
- Infusion and Injection Site Reactions: Possible
histamine-mediated symptoms have been reported with Micafungin for
Injection, including rash, pruritus, facial swelling, and
vasodilatation. Slow the infusion rate if infusion reaction occurs.
Injection site reactions, including phlebitis and thrombophlebitis
have been reported, at Micafungin for Injection doses of 50 to 150
mg/day. These reactions tended to occur more often in patients
receiving Micafungin for Injection via peripheral intravenous
administration.
- High Sodium Load: Each 50, 100, and 150 mL Galaxy container
contains 200, 400, and 600 mg of sodium, respectively. Avoid use in
patients with congestive heart failure, elderly patients, and
patients requiring restricted sodium intake.
- Adverse Reactions:
- Most common adverse reactions across adult and pediatric
clinical trials for all indications include diarrhea, nausea,
vomiting, abdominal pain, pyrexia, thrombocytopenia, neutropenia,
and headache.
- In pediatric patients younger than 4 months of age, the
following additional common adverse reactions were reported at an
incidence rate of ≥15%: hypokalemia, acidosis, sepsis, anemia, and
oxygen saturation decreased.
- Drug Interactions:
- Monitor for sirolimus, itraconazole or nifedipine toxicity, and
dosage of sirolimus, itraconazole or nifedipine should be reduced,
if necessary.
- Pregnancy: Based on animal data, Micafungin in Sodium Chloride
Injection may cause fetal harm. Advise pregnant women of the risk
to the fetus.
Please see accompanying full Prescribing Information for
Micafungin in 0.9% Sodium Chloride Injection.
Cyclophosphamide Injection
Indications
- Cyclophosphamide Injection is an alkylating drug indicated for
treatment of adult and pediatric patients with:
- Malignant Diseases: malignant lymphomas: Hodgkin's disease,
lymphocytic lymphoma, mixed-cell type lymphoma, histiocytic
lymphoma, Burkitt's lymphoma; multiple myeloma, leukemias, mycosis
fungoides, neuroblastoma, adenocarcinoma of ovary, retinoblastoma,
breast carcinoma.
Important Risk Information
- Contraindications
- Hypersensitivity: Cyclophosphamide is contraindicated in
patients who have a history of severe hypersensitivity reactions to
it, any of its metabolites, or to other components of the product.
Anaphylactic reactions including death have been reported. Possible
cross-sensitivity with other alkylating agents can occur.
- Urinary outflow obstruction
- Myelosuppression, Immunosuppression, Bone Marrow Failure and
Infections: Cyclophosphamide can cause myelosuppression, bone
marrow failure, and severe immunosuppression which may lead to
serious and sometimes fatal infections, including sepsis and septic
shock. Latent infections can be reactivated. Monitoring of complete
blood counts is essential during cyclophosphamide treatment so that
the dose can be adjusted, if needed.
- Urinary Tract and Renal Toxicity: Hemorrhagic cystitis,
pyelitis, ureteritis, and hematuria have been reported with
cyclophosphamide. Discontinue cyclophosphamide therapy in case of
severe hemorrhagic cystitis. Urotoxicity may require interruption
of cyclophosphamide treatment or cystectomy. Urotoxicity can be
fatal. Before starting treatment, exclude or correct any urinary
tract obstructions. Urinary sediment should be checked regularly
for the presence of erythrocytes and other signs of urotoxicity
and/or nephrotoxicity. Cyclophosphamide Injection should be used
with caution, if at all, in patients with active urinary tract
infections. Aggressive hydration with forced diuresis and frequent
bladder emptying can reduce the frequency and severity of bladder
toxicity. Mesna has been used to prevent severe bladder
toxicity.
- Cardiotoxicity: Myocarditis, myopericarditis, pericardial
effusion including cardiac tamponade, and congestive heart failure,
which may be fatal, have been reported with cyclophosphamide
therapy. Supraventricular arrhythmias and ventricular arrhythmias
have been reported after treatment with regimens that included
cyclophosphamide. The risk of cardiotoxicity may be increased with
high doses of cyclophosphamide, in patients with advanced age, and
in patients with previous radiation treatment to the cardiac region
and/or previous or concomitant treatment with other cardiotoxic
agents. Monitor patients, especially those with risk factors for
cardio toxicity or pre-existing cardiac disease.
- Pulmonary Toxicity: Pneumonitis, pulmonary fibrosis, pulmonary
veno-occlusive disease and other forms of pulmonary toxicity
leading to respiratory failure have been reported during and
following treatment with cyclophosphamide. Late onset pneumonitis
appears to be associated with increased mortality. Monitor patients
for signs and symptoms of pulmonary toxicity.
- Secondary Malignancies: Cyclophosphamide is genotoxic.
Secondary malignancies have been reported in patients treated with
cyclophosphamide-containing regimens. The risk of bladder cancer
may be reduced by prevention of hemorrhagic cystitis.
- Veno-occlusive Liver Disease (VOD): VOD including fatal outcome
has been reported in patients receiving cyclophosphamide-containing
regimens. A cytoreductive regimen in preparation for bone marrow
transplantation that consists of cyclophosphamide in combination
with whole-body irradiation, busulfan, or other agents has been
identified as a major risk factor. VOD has also been reported to
develop gradually in patients receiving long-term low-dose
immunosuppressive doses of cyclophosphamide.
- Alcohol Content: The alcohol content in a dose of
Cyclophosphamide Injection may affect the central nervous system.
Consideration should be given to the alcohol content on the ability
to drive or use machines immediately after the infusion.
- Embryo-Fetal Toxicity: Cyclophosphamide Injection can cause
fetal harm when administered to a pregnant woman. Exposure to
cyclophosphamide during pregnancy may cause birth defects,
miscarriage, fetal growth retardation, and fetotoxic effects in the
newborn. Advise females of reproductive potential to use effective
contraception during treatment and for up to 1 year after
completion of therapy. Advise male patients with female partners of
reproductive potential to use effective contraception during
treatment and for 4 months after completion of therapy.
- Infertility: Male and female reproductive function and
fertility may be impaired in patients being treated with
Cyclophosphamide Injection. Cyclophosphamide interferes with
oogenesis and spermatogenesis. It may cause sterility in both
sexes. Cyclophosphamide-induced sterility may be irreversible in
some patients.
- Adverse Reactions: Most common adverse reactions reported are
neutropenia, febrile neutropenia, fever, alopecia, nausea,
vomiting, and diarrhea.
- Lactation: Advise not to breastfeed.
- Renal Patients: Monitor for toxicity in patients with moderate
and severe renal impairment.
Please see accompanying full Prescribing Information for
Cyclophosphamide Injection.
Pantoprazole Sodium in 0.9% Sodium Chloride Injection
Indications
- Pantoprazole Sodium in 0.9% Sodium Chloride Injection is a
proton pump inhibitor (PPI) indicated in adults for the following:
- Short-term treatment (7 to 10 days) of gastroesophageal reflux
disease (GERD) associated with a history of erosive esophagitis
(EE).
- Pathological hypersecretion conditions including
Zollinger-Ellison (ZE) Syndrome.
Important Risk Information
- Contraindications
- Patients with a known hypersensitivity to any component of the
formulation or to substituted benzimidazoles. Hypersensitivity
reactions may include anaphylaxis, anaphylactic shock, angioedema,
bronchospasm, acute tubulointerstitial nephritis, and
urticaria.
- Patients receiving rilpivirine-containing products.
- Presence of Gastric Malignancy: In adults, symptomatic response
to therapy does not preclude the presence of gastric malignancy.
Consider additional follow-up and diagnostic testing in adult
patients who have a suboptimal response or an early symptomatic
relapse after completing treatment with a PPI. In older patients,
also consider an endoscopy.
- Injection Site Reactions: Thrombophlebitis was reported in
association with the administration of another intravenous
pantoprazole sodium product.
- Potential for Exacerbation of Zinc Deficiency: Pantoprazole
Sodium in 0.9% Sodium Chloride Injection contains edetate disodium
(the salt form of EDTA), a chelator of metal ions including zinc.
Therefore, zinc supplementation should be considered in patients
who are prone to zinc deficiency. Caution should be used when other
EDTA containing products are also co-administered
intravenously.
- Acute Tubulointerstitial Nephritis (TIN): Has been observed in
patients taking PPIs and may occur at any point during PPI therapy.
Patients may present with varying signs and symptoms from
symptomatic hypersensitivity reactions to non-specific symptoms of
decreased renal function. Discontinue Pantoprazole Sodium in 0.9%
Sodium Chloride Injection and evaluate patients with suspected
acute TIN.
- Clostridioides difficile-associated diarrhea: Published
observational studies suggest that PPI therapy may be associated
with an increased risk of Clostridioides difficile-associated
diarrhea, especially in hospitalized patients. This diagnosis
should be considered for diarrhea that does not improve. Patients
should use the lowest dose and shortest duration of PPI therapy
appropriate to the condition being treated.
- Bone Fracture: Several published observational studies suggest
that PPI therapy may be associated with an increased risk for
osteoporosis-related fractures of the hip, wrist, or spine. The
risk of fracture was increased in patients who received high-dose,
defined as multiple daily doses, and long-term PPI therapy (a year
or longer). Patients should use the lowest dose and shortest
duration of PPI therapy appropriate to the condition being treated.
Patients at risk for osteoporosis-related fractures should be
managed according to established treatment guidelines.
- Severe Cutaneous Adverse Reactions: Including erythema
multiforme, Stevens-Johnson syndrome (SJS), toxic epidermal
necrolysis (TEN), drug reaction with eosinophilia and systemic
symptoms (DRESS), and acute generalized exanthematous pustulosis
(AGEP) have been reported in association with the use of PPIs.
Discontinue Pantoprazole Sodium in 0.9% Sodium Chloride Injection
at the first signs or symptoms of severe cutaneous adverse
reactions or other signs of hypersensitivity and consider further
evaluation.
- Cutaneous Lupus Erythematosus (CLE) and Systemic Lupus
Erythematosus (SLE): Have been reported in patients taking PPIs,
including pantoprazole sodium. These events have occurred as both
new onset and an exacerbation of existing autoimmune disease. The
majority of PPI-induced lupus erythematous cases were CLE. Avoid
administration of PPIs for longer than medically indicated. If
signs or symptoms consistent with CLE or SLE are noted in patients,
discontinue the drug and refer the patient to the appropriate
specialist for evaluation. Most patients improve with
discontinuation of the PPI alone in 4 to 12 weeks.
- Hepatic Effects: Mild, transient transaminase elevations have
been observed in clinical studies with another intravenous
pantoprazole sodium product. The clinical significance of this
finding in a large population of subjects is unknown.
- Hypomagnesemia and Mineral Metabolism: Hypomagnesemia,
symptomatic and asymptomatic, has been reported rarely in patients
treated with PPIs for at least three months, and in most cases
after a year of therapy. Serious adverse events include tetany,
arrhythmias, and seizures. Hypomagnesemia may lead to hypocalcemia
and/or hypokalemia and may exacerbate underlying hypocalcemia in
at-risk patients. In most patients, treatment of hypomagnesemia
required magnesium replacement and discontinuation of the PPI.
- Fundic Gland Polyps: PPI use is associated with an increased
risk of fundic gland polyps that increases with long-term use,
especially beyond one year. Most PPI users who developed fundic
gland polyps were asymptomatic. Use the shortest duration of PPI
therapy appropriate to the condition being treated.
- Adverse Reactions: Most common adverse reactions (incidence
> 2%) are headache, diarrhea, nausea, abdominal pain, vomiting,
flatulence, dizziness, and arthralgia.
- Drug Interactions: See the full prescribing information for a
list of clinically important drug interactions.
- Pregnancy: Based on animal data, may cause fetal harm.
Please see accompanying full Prescribing Information for
Pantoprazole Sodium in 0.9% Sodium Chloride Injection.
Cefazolin in Dextrose Injection, USP
Indications
- Cefazolin in Dextrose Injection is a cephalosporin
antibacterial indicated for:
- Treatment of respiratory tract infections in adults and
pediatric patients for whom appropriate dosing with this
formulation can be achieved. Limitations of
Use: Injectable benzathine penicillin is considered the drug
of choice in treatment and prevention of streptococcal infections,
including the prophylaxis of rheumatic fever.
- Treatment of the following infections caused by susceptible
isolates of the designated microorganisms in adult and pediatric
patients for whom appropriate dosing with this formulation can be
achieved: Urinary tract infections; Skin and skin structure
infections; Biliary tract infections; Bone and joint infections;
Genital infections; Septicemia; Endocarditis.
- Perioperative prophylaxis in adults and pediatric patients aged
10 – 17 years old for whom appropriate dosing with this formulation
can be achieved.
To reduce the development of drug-resistant bacteria and
maintain the effectiveness of Cefazolin in Dextrose Injection and
other antibacterial drugs, Cefazolin in Dextrose Injection should
be used only to treat or prevent infections that are proven or
strongly suspected to be caused by bacteria.
Important Risk Information
- Contraindications: Hypersensitivity to Cefazolin or other
cephalosporin class antibacterial drugs, penicillins, or other
beta-lactams.
- Hypersensitivity Reactions to Cefazolin, Cephalosporins,
Penicillins, or Other Beta-lactams: Serious and occasionally fatal
hypersensitivity (anaphylactic) reactions have been reported in
patients receiving beta-lactam antibacterial drugs. Before therapy
with Cefazolin in Dextrose Injection, careful inquiry should be
made to determine whether the patient has had previous immediate
hypersensitivity reactions to cefazolin, cephalosporins,
penicillins, or carbapenems. Exercise caution if this product is to
be given to penicillin-sensitive patients because
cross-hypersensitivity among betalactam antibacterial drugs may
occur in up to 10% of patients with a history of penicillin
allergy. If an allergic reaction occurs, discontinue the drug.
- Seizures in Patients with Renal Impairment: Seizures may occur
particularly in patients with renal impairment when the dosage is
not reduced appropriately. Discontinue Cefazolin in Dextrose
Injection if seizures occur or make appropriate dosage adjustments
in patients with renal impairment. Anticonvulsant therapy should be
continued in patients with known seizure disorders
- Clostridioides difficile-associated Diarrhea (CDAD): May range
in severity from mild diarrhea to fatal colitis. CDAD must be
considered in all patients who present with diarrhea following
antibiotic use. If CDAD is suspected or confirmed, ongoing
antibiotic use not directed against C. difficile may need to be
discontinued. Appropriate fluid and electrolyte management, protein
supplementation, antibiotic treatment of C. difficile, and surgical
evaluation should be instituted as clinically indicated.
- Prothrombin Activity: Cefazolin in Dextrose Injection may be
associated with a fall in prothrombin activity. Those at risk
include patients with renal or hepatic impairment or poor
nutritional state, as well as patients receiving a protracted
course of antimicrobial therapy, and patients previously stabilized
on anticoagulant therapy. Prothrombin time should be monitored in
patients at risk and exogenous vitamin K administered as
indicated.
- Adverse Reactions: Adult and Pediatric
Patients: Most common adverse reactions: gastrointestinal
(nausea, vomiting, diarrhea), and allergic reactions (anaphylaxis,
urticaria, skin rash). Pediatric Patients
with Perioperative Prophylaxis: The most frequently reported
adverse reactions (incidence ≥ 5%) were nausea, infusion site pain,
and headache.
- Drug Interactions:
- Probenecid: The renal excretion of cefazolin is inhibited by
probenecid. Co-administration of probenecid with Cefazolin in
Dextrose Injection is not recommended.
Please see accompanying full Prescribing Information for
Cefazolin in Dextrose Injection, USP.
Levetiracetam in Sodium Chloride Injection
Indications
- Levetiracetam in Sodium Chloride Injection is indicated for
adjunct therapy in adults (≥16 years of age) with the following
seizure types when oral administration is temporarily not feasible:
- Partial-onset seizures
- Myoclonic seizures in patients with juvenile myoclonic
epilepsy
- Primary generalized tonic-clonic seizures
Important Risk Information
- Contraindications: Levetiracetam in Sodium Chloride Injection
is contraindicated in patients with a hypersensitivity to
levetiracetam. Reactions have included anaphylaxis and
angioedema.
- Psychiatric Reactions: Behavioral abnormalities including
psychotic symptoms, suicidal ideation, irritability, and aggressive
behavior have been observed. Monitor patients for psychiatric signs
and symptoms.
- Somnolence and Fatigue: Monitor patients for these symptoms and
advise patients not to drive or operate machinery until they have
gained sufficient experience on levetiracetam.
- Anaphylaxis and Angioedema: Levetiracetam can cause anaphylaxis
or angioedema. In some reported cases, reactions were
life-threatening and required emergency treatment. If a patient
develops signs or symptoms of anaphylaxis or angioedema,
levetiracetam should be discontinued and the patient should seek
immediate medical attention.
- Serious Dermatological Reactions: Serious reactions, including
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis
(TEN), have been reported in patients treated with levetiracetam.
Recurrence of the serious skin reactions following rechallenge has
also been reported. Levetiracetam should be discontinued at the
first sign of a rash, unless the rash is clearly not drug-related.
If signs or symptoms suggest SJS/TEN, use of this drug should not
be resumed, and alternative therapy should be considered.
- Drug Reaction with Eosinophilia and Systemic Symptoms
(DRESS)/Multiorgan Hypersensitivity: This has been reported in
patients taking antiepileptic drugs, including levetiracetam. These
events can be fatal or life-threatening, particularly if diagnosis
and treatment do not occur as early as possible. DRESS typically,
although not exclusively, presents with fever, rash,
lymphadenopathy, and/or facial swelling, in association with other
organ system involvement, sometimes resembling an acute viral
infection. If such signs or symptoms are present, the patient
should be evaluated immediately. Levetiracetam should be
discontinued if an alternative etiology for the signs or symptoms
cannot be established.
- Coordination Difficulties: Monitor for ataxia, abnormal gait,
and incoordination. Patients should be monitored for these signs
and symptoms and advised not to drive or operate machinery until
they have gained sufficient experience on levetiracetam.
- Withdrawal Seizures: Levetiracetam must be gradually withdrawn.
But if withdrawal is needed because of a serious adverse reaction,
rapid discontinuation can be considered.
- Hematologic Abnormalities: Hematologic abnormalities occurred
in clinical trials and included decreases in white blood cell,
neutrophil, and red blood cells counts; decreases in hemoglobin and
hematocrit; and increases in eosinophil counts. Cases of
agranulocytosis, pancytopenia, and thrombocytopenia have been
reported in the post-marketing setting. A complete blood count is
recommended in patients experiencing significant weakness, pyrexia,
recurrent infections, or coagulation disorders.
- Adverse Reactions: Most common adverse reactions (incidence in
levetiracetam-treated patients is ≥5% more than in placebo-treated
patients) include: somnolence, asthenia, infection, and
dizziness.
- Pregnancy: Plasma levels of levetiracetam may be decreased;
monitor closely during pregnancy. Based on animal data, may cause
fetal harm. Encourage women who are taking levetiracetam injection
during pregnancy to enroll in the North American Antiepileptic Drug
(NAAED) pregnancy registry.
- Renal Impairment: Dosage adjustment is recommended for patients
with impaired renal function and supplemental doses should be given
to patients after dialysis.
Please see accompanying full Prescribing Information for
Levetiracetam in Sodium Chloride Injection.
This release includes forward-looking statements concerning
Micafungin in 0.9% Sodium Chloride Injection, Cyclophosphamide
Injection, Pantoprazole Sodium in 0.9% Sodium Chloride Injection,
Cefazolin in Dextrose Injection, USP and Levetiracetam in Sodium
Chloride Injection, including potential benefits associated with
the use of these products. The statements are based on assumptions
about many important factors, including the following, which could
cause actual results to differ materially from those in the
forward-looking statements: demand for and market acceptance for
new and existing products; product development risks; inability to
create additional production capacity in a timely manner or the
occurrence of other manufacturing or supply difficulties (including
as a result of natural disasters, public health crises and
epidemics/pandemics, regulatory actions or otherwise); satisfaction
of regulatory and other requirements; actions of regulatory bodies
and other governmental authorities; product quality, manufacturing
or supply, or patient safety issues; changes in law and
regulations; and other risks identified in Baxter's most recent
filing on Form 10-K and Form 10-Q and other SEC filings, all of
which are available on Baxter's website. Baxter does not undertake
to update its forward-looking statements.
Baxter is a registered trademark of Baxter International
Inc.
1 Includes line extensions.
2 Mercaldi CJ, Lanes S, Bradt J. Comparative risk of bloodstream
infection in hospitalized patients receiving intravenous medication
by open, point-of-care, or closed delivery systems. Am J
Health-Syst Pharm. 2013;70:957-965.
3 Billstein-Leber M, Carrillo CJD, Cassano AT, Moline K,
Robertson JJ. ASHP Guidelines on Preventing Medication Errors in
Hospitals. Am J Health Syst Pharm. 2018;75(19):1493-1517.
US-PH121-240011 (v3.0) 12/2024
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241211980642/en/
Media Contact Tara Reardon, (224) 948-5353
media@baxter.com
Investor Contact Clare Trachtman, (224) 948-3020
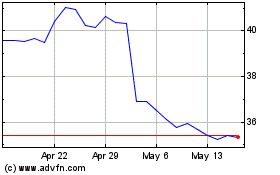
Baxter (NYSE:BAX)
Historical Stock Chart
From Dec 2024 to Dec 2024
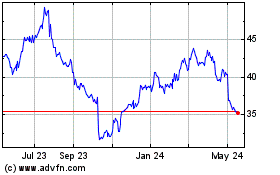
Baxter (NYSE:BAX)
Historical Stock Chart
From Dec 2023 to Dec 2024